
views
X
Research source
It's caused by repetitive thigh muscle contraction, which causes the patellar (kneecap) tendon to pull on the developing shinbone (tibia) creating inflammation and pain — and typically a visibly swollen bump. OSD occurs most often in boys, particularly those who play sports involving lots of running, jumping and sudden changes of direction — such as soccer and basketball.[2]
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
OSD is usually self limiting and only rarely causes permanent problems or disability.[3]
X
Research source
However, there are many ways to reduce the pain of OSD and make it more bearable until the condition resolves itself.
Using Home Care Remedies

Rest and avoid pain-inducing activities. Probably the most important action you can take to help alleviate the pain from OSD is to stop playing the sport or doing the activity that is contributing most to the problem. Sports that involve a lot of jumping, such as basketball and volleyball, are particularly bad for OSD. The amount of rest needed varies widely and depends on the person, but expect anywhere from a few weeks to a few months before a significant reduction in pain and swelling is noticed. Pain with OSD can be sporadic or nearly constant; it usually occurs in just one knee, but sometimes develops in both.

Apply ice to your knee. The application of ice is an effective treatment for essentially all acute musculoskeletal injuries, including OSD. Cold therapy should be applied to the inflamed bump (tibial tuberosity) just below your kneecap for 20 minutes every two to three hours for a couple of days, then reduce the frequency as the pain and swelling subside. Always wrap ice or frozen gel packs in a thin towel in order to prevent frostbite on your skin. If you don't have any ice or gel packs, then use a frozen bag of peas from your freezer.

Use a knee brace or patellar immobilizer. While resting and applying ice to your knee, consider also using a special knee brace or kneecap immobilizer while having to walk in order to take the stress off your patellar tendon. Knee braces can be found at stores that sell rehabilitation and medical supplies — ask a physical therapist, physician, or chiropractor for more info. Alternatively, you can try a patellar tendon strap, which fits around your leg just below your kneecap. It can support your kneecap's tendon during physical activity and distribute some of the force away from the tibial tuberosity. Complete inactivity is not necessary with OSD, but consider switching to other fun activities that don't involve jumping or running, such as swimming, rowing or golf.

Take anti-inflammatories or painkillers. Non-steroidal anti-inflammatories (NSAIDs) such as ibuprofen, naproxen or aspirin can be short-term solutions to help you deal with the pain and inflammation of OSD. Alternatively, you can try over-the-counter analgesics (painkillers) such as acetaminophen (Tylenol). These medications can be hard on your stomach, kidneys and liver, so it's best not to use them for more than 2 weeks at a stretch. Check with your doctor before taking any medications. Keep in mind that NSAIDs do not shorten the course of OSD. Steroids such as cortisone have powerful anti-inflammatory properties, but injections should not be given to adolescents with OSD due to the risk factors — mainly, potential tendon weakening, local muscle atrophy and reduced immune system function.

Stretch your quadriceps. Once the acute knee pain has settled down, start doing some quadriceps stretching. One of the causes of OSD is repetitive quadriceps contractions (from too much jumping, for example) and also overly tight quadricep tendons. As such, learning how to stretch this muscle group may help reduce the tension and inflammation in the area where the kneecap's tendon attaches to the upper shinbone (tibia). To stretch your quadriceps while standing, bend your leg behind you so your knee is bent, your heel about at the level of your butt. Grab your ankle and pull your foot toward your body until you feel a nice stretch in your lower thigh and knee. Hold for about 30 seconds and repeat three to five times daily until you notice reduced symptoms. Stretches for the hamstrings, which are also commonly tight, may also be performed. Bending over at the waist and trying to touch your toes is a good basic hamstring stretch.
Using Alternative Therapies

Get a leg massage. A deep tissue massage is helpful for mild-to-moderate strains because it reduces muscle tension, combats inflammation and promotes relaxation. Start with a 30 minute massage, focusing on your thigh muscles and kneecap area. Allow the therapist to go as deep as you can tolerate without wincing. The therapist may use a focal cross-friction technique on your kneecap area if they think there's a build-up of scar tissue. Always drink lots of water immediately following a massage in order to flush out inflammatory by-products and lactic acid from your body. Failure to do so might cause a headache or mild nausea.
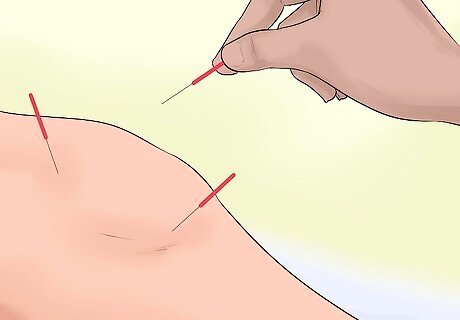
Try acupuncture. Acupuncture involves sticking thin needles into specific points on the body to reduce pain and inflammation. Acupuncture is not commonly recommended for OSD, but it's virtually risk-free and certainly worth a try, especially if it's done when the symptoms first occur. Based on the principles of traditional Chinese medicine, acupuncture works by releasing a variety of substances including endorphins and serotonin, which act to reduce pain. Acupuncture points that may provide relief to your knee pain are not all located near where the pain is — some can be in distant areas of your body. Acupuncture is practiced by a variety of health professionals including some physicians, chiropractors, naturopaths, physical therapists and massage therapists — whoever you choose should be certified by the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM).
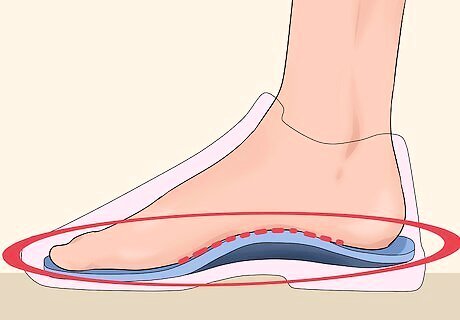
Consider shoe orthotics. A risk factor for OSD is poor biomechanics while running and jumping, and sometimes that's caused by flat feet and knock-kneed posture. Orthotics are customized shoe inserts that support the arch of your foot, align your legs and promote better biomechanics while standing, walking, running and jumping. Health professionals who make custom orthotics include podiatrists and some osteopaths and chiropractors. Some health insurance plans cover the cost of customized orthotics, but if yours doesn't, then consider a pair of off-the-shelf insoles — they're considerably less expensive and may provide quick relief.
Getting Medical Treatment

Try therapeutic ultrasound treatments. Therapeutic ultrasound is a treatment used by some physicians, chiropractors and physical therapists in order to reduce inflammation and stimulate healing for a variety of injuries, including OSD. Like its name infers, it emits sound frequencies through crystals (you can't hear it) that positively impact cells and tissues of the body. Although a single ultrasound treatment can sometimes completely relieve your pain and inflammation, more than likely it will take three to five treatments to notice significant results. Therapeutic ultrasound treatments are painless and usually last 10 – 20 minutes.

Seek out some physiotherapy. If your OSD is not responding to home care or alternative therapies, then consider getting some physiotherapy for your knee. A physical therapist can show you specific and tailored stretches and strengthening exercises for your quadriceps and knee. Physiotherapy is usually required two to three times per week for four to eight weeks to positively impact chronic musculoskeletal problems. A physical therapist can also treat your knee with therapeutic ultrasound, maybe even tape your patella and possibly also make you a pair of custom orthotics.
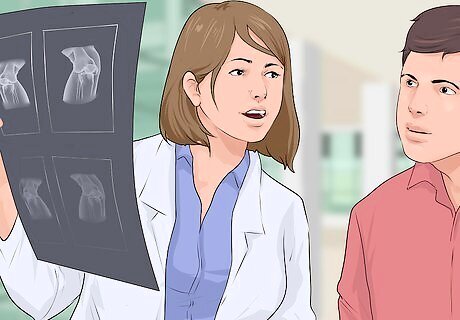
See a medical specialist. You may need to see a medical specialist such as an orthopedist or rheumatologist in order to rule out more serious causes of knee pain that can mimic OSD — conditions like a patellar or tibial stress fracture, bone infection, inflammatory arthritis, bone tumor, osteochondritis dissecans or Perthes disease. X-rays, bone scans, diagnostic ultrasound, MRI and CT scans are tools that specialists may use to help diagnose your knee pain. Your doctor may also send you for a blood test to rule out rheumatoid arthritis or a bone infection.















Comments
0 comment