
views
A study shows how SARS-COV-2 infects brain cells called astrocytes, causing structural changes in the brain. Infection with SARS-CoV-2 can cause brain alterations and neurocognitive dysfunction, particularly in long COVID-19 syndrome, but the underlying mechanisms are elusive.
Daniel Martins-de-Souza and colleagues used MRI to compare brain structure in 81 study participants recovering from a mild COVID-19 infection and 81 healthy individuals. The authors found that the former group exhibited reduced cortical thickness, which was correlated with cognitive impairments and symptoms such as anxiety and depression.
The authors analyzed brain samples from 26 people who had died of COVID-19, finding that samples from five of these individuals exhibited tissue damage.
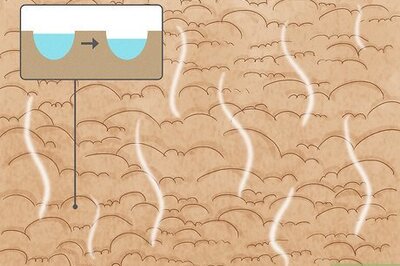
Further analysis of damaged brain samples revealed that astrocytes, which are brain cells that sustain neuronal metabolism, were particularly likely to be infected with SARS-CoV-2 and that the virus enters these cells through the NRP1 receptor.
Once infected, astrocytes exhibited altered levels of metabolites used to fuel neurons and neurotransmitter production, and the infected cells secreted neurotoxic molecules. According to the authors, the findings uncover structural changes observed in the brains of people with COVID-19.
The significance of the study denotes the neurological symptoms that are among the most prevalent of the extrapulmonary complications of COVID-19, affecting more than 30 per cent of patients. In this study, we provide evidence that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is found in the human brain, where it infects astrocytes and to a lesser extent, neurons.
We also show that astrocytes are susceptible to SARS-CoV-2 infection through a noncanonical mechanism that involves spike-NRP1 interaction and respond to the infection by remodeling energy metabolism, which in turn, alters the levels of metabolites used to fuel neurons and support neurotransmitter synthesis. The altered secretory phenotype of infected astrocytes then impairs neuronal viability. These features could explain the damage and structural changes observed in the brains of COVID-19 patients.
Although increasing evidence confirms neuropsychiatric manifestations associated mainly with severe COVID-19 infection, long-term neuropsychiatric dysfunction (recently characterized as part of “long COVID-19” syndrome) has been frequently observed after mild infection.
The study shows the spectrum of cerebral impact of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, ranging from long-term alterations in mildly infected individuals (orbitofrontal cortical atrophy, neurocognitive impairment, excessive fatigue and anxiety symptoms) to severe acute damage confirmed in brain tissue samples extracted from the orbitofrontal region (via endonasal transethmoidal access) from individuals who died of COVID-19.
In an independent cohort of 26 individuals who died of COVID-19, we used histopathological signs of brain damage as a guide for possible SARS-CoV-2 brain infection and found that among the 5 individuals who exhibited those signs, all of them had genetic material of the virus in the brain.
Brain tissue samples from these five patients also exhibited foci of SARS-CoV-2 infection and replication, particularly in astrocytes. Supporting the hypothesis of astrocyte infection, neural stem cell-derived human astrocytes in vitro are susceptible to SARS-CoV-2 infection through a noncanonical mechanism that involves spike-NRP1 interaction.
SARS-CoV-2-infected astrocytes manifested changes in energy metabolism and in key proteins and metabolites used to fuel neurons, as well as in the biogenesis of neurotransmitters. Moreover, human astrocyte infection elicits a secretory phenotype that reduces neuronal viability.
The study results in cognitive Impairments and Neuropsychiatric Symptoms in Convalescent COVID-19 Patients Correlate with Altered Cerebral Cortical Thickness. A cortical surface-based morphometry analysis (using a high-resolution 3T MRI) on 81 subjects diagnosed with mild COVID-19 infection (62 self-reported anosmias or dysgeusia) who did not require oxygen support (methodological details and patient demographics are presented in SI Appendix).
The analysis was performed within an average (SD) interval of 57 (26) d after SARS-CoV-2 detection by qRT-PCR, and the subjects were compared with 81 healthy volunteers (without neuropsychiatric comorbidities) scanned during the COVID-19 pandemic (balanced for age [P = 0.97] and sex [P = 0.3]). The COVID-19 group presented higher levels of anxiety and depression symptoms, fatigue, and excessive daytime sleepiness (SI Appendix, Table S1 shows epidemiological and clinical data).
An analysis of cortical thickness (adjusted for multiple comparisons using the Holm-Bonferroni method) revealed areas of reduced cortical thickness exclusively in the left hemisphere, including the left gyrus rectus (P = 0.01), superior temporal gyrus (P = 0.036), inferior temporal sulcus (P = 0.02), and posterior transverse collateral sulcus (P = 0.003) (Fig. 1A). There was no observed increase in cortical thickness.
Read the Latest News and Breaking News here














Comments
0 comment