views
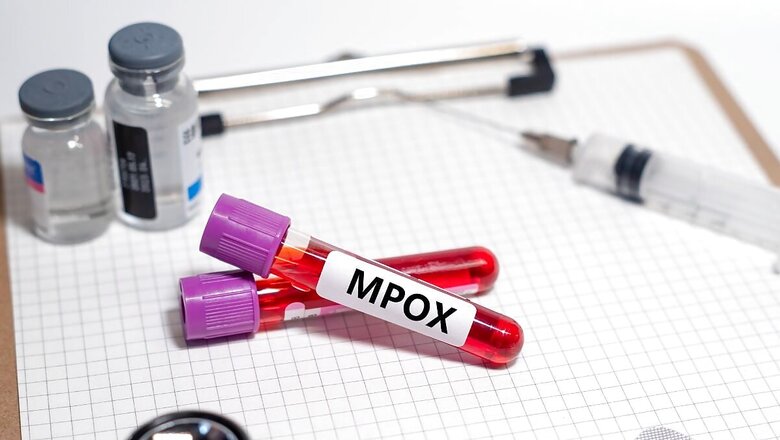
The re-emergence of Mpox is causing ripples, maybe, because we all are still grappling with lingering anxiety from Covid-19. The facts, however, may help ease concerns.
A similar warning was issued in 2022 following a global outbreak, but it was revoked as new cases declined sharply in 2023. Mpox, which shares some similarities with smallpox, was first identified in humans in 1970 in the Democratic Republic of Congo. The disease was primarily endemic to Central and West Africa, with two major types or clades identified.
The viral infection causes fever, headache, rashes, pus-filled lesions and flu-like symptoms, which are usually mild but, in some cases, they can cause death as well. In this episode of Health Matters, let’s understand how we can fight against Mpox, what steps we can take if the situation worsens and what we still need to know more.
Current status of Mpox
Currently, the cases are surging in the Democratic Republic of Congo and spreading beyond its borders. So far, more than 96 per cent of all cases and deaths are in a single country — Congo. The global health agency said Mpox was recently identified for the first time in four East African countries where all of the outbreaks were linked to the epidemic in Congo.
WHO warned further that imported cases of the new and more dangerous strain in Europe were likely as Sweden has also announced infection.
Sweden has reported a case caused by Clade I — the first case to be diagnosed outside the African continent, clearly reflecting the spread of the virus. Later, Pakistan identified three patients with the Mpox virus.
Will we be able to survive the comeback?
Going by the availability of vaccines and medicine, it seems the world will be able to get through this attack.
The previous attacks of Mpox were due to Clade IIB but, this time, the fear is Mpox Clade IB. This clade, perhaps, has a higher rate of transmission. However, experts are not yet sure as the pool of patients is still small and adequate studies have not been done.
While its transmissibility and lethality are yet to be proven, one significant advantage of Clade IB is that it manifests lesions that are visible on the whole body. The skin boils and lesions can appear on general skin and areas such as near the oral cavity, unlike Clade IIB where skin boils appear mainly near the genitals. This can make screening at airports and seaports easy if done efficiently.
Also, two vaccines are already available for reducing the risk and severity of Mpox infection — Jynneos and Acam2000.
The world also has a medicine called Tecovirimat which is an antiviral medication that was generally stockpiled during the wave of smallpox. The medicine was approved by the United States in 2018 as it was the first drug specifically for treating poxviruses.
Manufacturing of Tecovirimat can be ramped up easily, as per experts. Additionally, countries like India need to train healthcare staff to distinguish between boils and skin lesions caused by Mpox, chickenpox, and other infections.
One of the biggest challenges for India is to fight the stigma attached to Mpox — a disease known to be transmitted sexually.
During the Clade II Mpox outbreak in 2022, the main transmission route was associated with sexual activity among certain gay, bisexual, and other men who have sex with men (MSM). Here, this may prevent people from coming out and visiting doctors despite noticing the symptoms.
Otherwise, experts believe that management of the disease is quite easy as it involves an isolation period of two to three weeks with minimal chances of spreading to family members. It only requires catching the symptoms on time and taking the advice of healthcare professionals. The disease may become slightly tricky for those who already have other health conditions. Also, those who have had a shot of small pox vaccines are assumed to be safe from this virus.
Fear is that the virus could be evolving
Experts told News18 that Clade I, seen in the Congo basin, had less human-to-human spread but led to a higher rate of severe infections and death. Clade II, seen in West Africa, had a greater spread but infections were less severe. The large international surge starting July 2022, primarily driven by sexual contact amongst men, was due to Clade IIB, with even lower virulence.
The 2022 MPox outbreak was thus mostly a self-limited disease, with low mortality rates. Despite this, there were about 200 deaths, mostly in countries that had never reported Mpox before.
The current outbreak appears to be distinct, involving Clade I. Cases are being reported in multiple countries surrounding DRC, with most fatalities occurring in children, raising concerns about possible non-sexual human-to-human transmission.
WHO data shows a total of 548 people have died of which an estimated 463 were children. Virologists believe that the virus might be evolving. Hence, efforts must focus on containing the ongoing spread of Mpox and closely monitoring the evolution of the virus.
Is the virus becoming more powerful, or will it just fizzle out like it has in the past? Humans are striving to stay ahead of the virus, but the virus seems to be racing to outpace our efforts. Here’s to hoping that we can ultimately win the race.

















Comments
0 comment