
views
Using Aloe Vera to Treat Rheumatoid Arthritis

Learn about aloe vera gel and juice. Gel from the aloe vera plant is a traditional treatment for wounds, burns, infections, and some kinds of joint pain and arthritis. You can use it directly on the joints or drink aloe vera juice to decrease inflammation. Aloe vera may be useful for RA because of its anti-inflammatory properties, its property as a pain-reliever (likely due to the anti-inflammatory properties), and in speeding up wound healing. It is also a safe moisturizing and anti-aging agent. The gel comes from the central part of the aloe leaf, known as the "inner fillet." It contains larger complex sugars than aloe juice does. These complex sugars are thought to be responsible for the benefits of aloe. The juice is extracted from the outer leaves and also contains complex sugars.

Get aloe vera gel out of the plant. If you have a mature aloe plant, cut off a leaf using a pair of sharp scissors and peel away the outer leaf to reveal the clear gel inside. Use your fingers to get the gel out or cut the end off the leaf and squeeze the gel out. If you want to purchase the gel, check online or at your local health food store. Buy organic aloe vera with no additives or preservatives.

Apply aloe vera gel to your joints. At first, apply the aloe to a small area to test for any possible reactions. If a rash or other problems develop, stop using it. If there's no skin irritation, spread the gel onto the areas that are bothering you the most. Apply it like you would any other lotion. This will give you temporary relief from the pain of rheumatoid arthritis. As long as there's no skin irritation, you can keep treating the pain with aloe vera as long as you want. Most people don't experience side effects, but aloe may cause redness, a burning or a stinging sensation and rarely, a short-term rash.
Learn about aloe vera juice's side effects and health interactions. Aloe vera juice has been reported to decrease immune responses, which may be helpful in RA. Drinking aloe vera juice can cause cramping, diarrhea and gas. If this happens, stop drinking it. Drinking aloe vera juice can lower blood sugar and interfere with diabetes medications, so don't drink the juice for more than 3 to 4 weeks. It can also decrease the absorption of steroid creams, and decrease potassium levels if you drink the juice. Always talk to a knowledgeable healthcare professional before combining any medications with supplements, including topical or oral aloe vera. While there are no long-term studies of internal aloe vera's effects, one study found a link between the juice and colon cancer. The Center for Science in the Public Interest (CSPI) does not recommend drinking aloe vera. But, it strongly recommends using aloe vera topically.
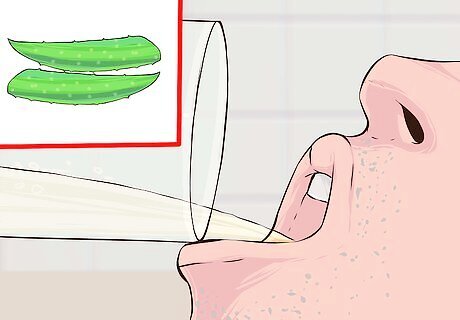
Drink aloe vera juice. Look for organic aloe vera juice (like Lily of the Desert or Nature's Way) with no additives or preservatives. Start with small amounts, like 2–3 fluid ounces (59–89 mL) once a day, to see how you react to the juice. Work your way up to 2–3 fluid ounces (59–89 mL) 3 times a day. It does taste a little bitter and may take some getting used to. You can try adding 1 teaspoon (4.9 mL) of honey to the juice or mix it with a fruit juice until you like the flavor. Never drink the gel, since it contains a strong laxative and can cause diarrhea.
Changing Your Diet and Lifestyle
Choose higher-quality foods for your diet. Try to eat mainly organic foods. These contain no pesticides or other chemicals, like hormones and antibiotics, which may be related to an increased risk of inflammation. You should also limit the amount of processed and pre-packaged food you eat. This will limit additives and preservatives that may cause increased inflammation in some people. This will also ensure you're eating complex carbohydrates, not simple carbs, which can increase levels of inflammation. Try to cook from scratch, using whole foods. This will preserve most of the vitamins, minerals, and nutrients. A rule of thumb is that if the food is too white—like white bread, white rice, or white pasta—it has been processed. Instead, eat whole grain breads, brown rice, and whole grain pasta.

Eat more fruits and vegetables. Aim for 2/3 of your total diet coming from fruits, vegetables, and whole grains. Fruits and vegetables have high levels of antioxidants which might decrease inflammation. Try to choose fresh produce. Frozen can also be used, but you should avoid eating vegetables in any sort of fattening, creamy sauce. Avoid fruits that have sugar or heavy syrup. Instead, choose brightly colored fruits and vegetables with lots of antioxidants. These include: Berries (blueberries and raspberries) Apples Plums Oranges Citrus Leafy green vegetables Winter and Summer squash Bell peppers
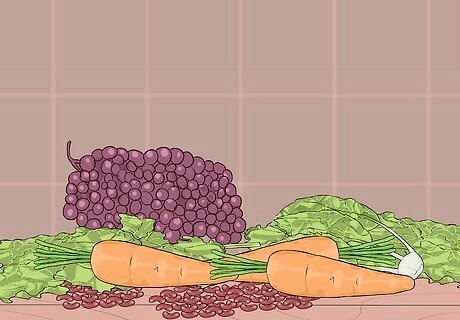
Eat more fiber. Fiber can decrease inflammation. Try to make sure you're getting a minimum of 20-35 grams of fiber daily. High-fiber foods include whole grains, fruits, vegetables, beans and legumes, and seeds. The following are great sources of fiber: Brown rice, bulgur wheat, buckwheat, oats, millet, quinoa Apples, pears, figs, dates, grapes, berries of all kinds Leafy green vegetables (spinach, mustard, collard, Swiss chard, kale), carrots, broccoli, brussels sprouts, bok choy, beets Peas, lentils, all beans (kidney, black, white, lima) Pumpkin seeds, sesame seeds, sunflower seeds, and nuts, including almonds, pecans, walnuts and pistachio nuts

Limit the amount of red meat you eat. If you do eat meats, make sure the beef is lean (preferably grass fed since it has the natural ratio of omega-3 and omega-6 fats), and the poultry is skinless. Any meat you eat should be raised without hormones or antibiotics and you should trim the fat. Limiting meat will help reduce your saturated fat intake, something the American Heart Association recommends that you limit to less than 7% of your total daily calories. You can avoid saturated fats by not using butter, margarine, and shortening in your cooking. Instead, use olive or canola oils. The AHA also recommends that you avoid all trans fats. Read food labels and avoid any that have "partially hydrogenated fats." This means the product has trans fats, even if the label says "0 trans fats."
Include more fish in your diet. Fish is good quality protein and has good amounts of the healthier omega-3 fats. Higher omega-3 fat intake is associated with a decreased level of inflammation. Fish with higher levels of omega-3 fats include salmon, tuna, trout, sardines, and mackerel. Don't forget to drink plenty of water and stay hydrated.
Add anti-inflammatory spices and herbs to your food. Certain spices and herbs can reduce the pain associated with rheumatoid arthritis inflammation. Several of these exist as supplements (garlic, turmeric/curcumin, omega-3 fatty acids, and vitamin C and E), but be sure to talk to your doctor before taking them. It's better to get them from your diet, rather than supplements. These herbs and spices include: Garlic Turmeric/Curcumin Basil Oregano Cloves Cinnamon Ginger Chili peppers

Engage in moderate exercise. Exercise can help maintain your overall health and strong muscles and bones. A physical therapist can help you determine the most beneficial type of exercise. But, don't forget that exercise can mean low-impact activities like aerobics, weigh training, walking, hiking, Tai Chi, or yoga. All these can help maintain strength and flexibility. Be sure to balance rest and exercise. If you have a rheumatoid arthritis flare up, it's more helpful to take a short break instead of prolonged bed rest.
Take disease-modifying antirheumatic drugs (DMARDs). These include anti-inflammatory agents. Your doctor may also prescribe antibodies made against tumor necrosis factor. It's not clear how these drugs function in rheumatoid arthritis, but they're usually used alongside anti-inflammatory drugs. Or, you may also be prescribed a newer agent, biologics which are human genetically engineered proteins, combined with anti-inflammatory agents. Nonsteroidal anti-inflammatory drugs and analgesics are used along with other medications. DMARDs, like methotrexate, can cause serious liver injury and hypersensitivity reactions. Other side effects can include fever, fatigue, cough, and trouble breathing.
Understanding Rheumatoid Arthritis

Watch for the symptoms of rheumatoid arthritis. The first signs and symptoms are tender and swollen joints that often feel warm to the touch. Many people with rheumatoid arthritis have relatively mild pain and stiffness but experience periodic “flare ups” where the signs and symptoms get worse. Other people have constant, chronic symptoms. As the disease progresses, joints and bones can become damaged, leading to increasing loss of function, although early treatment can limit the damage. Other symptoms may include: Fatigue, muscle pain, and general stiffness that lasts at least 1 hour after waking or after a long rest period (unlike the pain and stiffness of osteoarthritis, which dissipates faster). Suffering from other disorders more frequently than those without the disease. These may include other autoimmune diseases (like Sjogren's Syndrome), vasculitis (an inflammation of the blood vessels), anemia (lower than normal numbers of red blood cells that carry oxygen to tissues), and lung disease. Rheumatoid nodules, which develop in up to 35% of individuals with rheumatoid arthritis. The nodules show up as bumps under the skin near the affected joint, most commonly near the elbows. They're not usually painful, are freely movable under the skin, and can range in size from a pea up to the size of a lemon.

Understand the risk factors for getting rheumatoid arthritis. While the cause of rheumatoid arthritis isn't known, it seems to be linked to genetic factors. It's likely that inheriting a group of genes, not a single gene, increases your risk of rheumatoid arthritis. Hormones and environmental factors also play a role in developing the disease. Men and women of any race or ethnic background can get rheumatoid arthritis, but it occurs in women more frequently than in men. Women are about 2 to 3 times more likely to get the disease, which most often begins in middle age.

Learn how rheumatoid arthritis is diagnosed. Rheumatoid arthritis is diagnosed using your signs, symptoms, medical and family history along with a physical exam. Your doctor will then use the diagnosis to create a treatment plan, with the primary goal being reduction of the pain by reducing inflammation and minimizing any damage to the joints. To diagnose rheumatoid arthritis, your doctor will do: Lab tests, including x-rays or other imaging of the affected joints Blood samples, specifically one to examine blood for Rheumatoid Factor (RF) and other non-specific tests. The RF test can diagnose rheumatoid arthritis, while the non-specific ones indicate underlying inflammation. Diagnostic tests to rule out other conditions that mimic rheumatoid arthritis, such as infectious arthropathies (painful joints from infection), Systemic Lupus Erythematosus (SLE), ankylosing spondylitis (which primarily affect the spine and larger joints), and fibromyalgia.
When to Seek Medical Care
Make an appointment with your doctor as soon as you notice arthritis symptoms. Rheumatoid arthritis can lead to a variety of other health problems if you don’t manage it with proper medical care. If you suspect you have rheumatoid arthritis, see your doctor right away so they can diagnose your condition and recommend an appropriate treatment. You should see a doctor any time you have persistent pain or swelling in your joints. Possible serious complications of untreated rheumatoid arthritis include osteoporosis, infections, carpal tunnel syndrome, heart problems (such as hardened or blocked arteries), and lung disease.
Develop a care plan with your doctor and follow it closely. Once your doctor diagnoses you with rheumatoid arthritis, they can make recommendations for managing your condition safely and effectively. They may also refer you to other specialists, such as rheumatologists or physical therapists, who have experience treating RA. Talk to your doctor and the rest of your care team to make sure you understand their care instructions. In addition to making healthy lifestyle changes, your care team may recommend using medications (such as DMARDs and anti-inflammatory drugs), physical or occupational therapy, and surgical treatments (such as tendon repair or joint replacement) to manage your RA.
Get checkups as frequently as your doctor recommends. Rheumatoid arthritis is a disease that can be managed, but there’s currently no cure. You’ll need to check in with your doctor frequently to make sure that the treatments they recommend are working and that no new complications have developed. Ask your doctor how often you need to come in for regular checkups. They may recommend coming in every 1-2 months. Research shows that frequent checkups (i.e., between 7 and 11 times per year) are associated with better treatment results for patients with RA than less frequent checkups (fewer than 7 per year).
Let your doctor know if you experience new symptoms. Even if you are already receiving medical care for your rheumatoid arthritis, sometimes your condition might change or worsen unexpectedly. If this happens, make an appointment with your doctor right away, even if you’re not due for a checkup. For example, see your doctor if you notice increasing pain and swelling, changes in the appearance of your joints, or symptoms of related health problems (such as shortness of breath due to damage in the lungs).




















Comments
0 comment