
views
X
Trustworthy Source
Cleveland Clinic
Educational website from one of the world's leading hospitals
Go to source
Many medications and lifestyle changes can help your body be more sensitive to insulin, which can help if you have type 2 diabetes. However, if low insulin is the problem, you may need to take medications to increase the level of insulin in your body.
Medications

Take medication that improves insulin sensitivity. Metformin is usually the first medicine prescribed for diabetes. It reduces the amount of sugar your liver produces and improves how your body uses the insulin you have. If you need further medical help to lower your blood sugar, your doctor may try a medication like Avandia or Actos – though these can have serious side effects. Often a combination of medications with different effects on the body will be used to simultaneously increase the insulin you make, improve how you use insulin, and lower your blood sugar in other ways.

Ask your doctor if you should take insulin directly. When lifestyle and medications don’t control your blood sugar, you may need to take insulin directly. There are long-acting and short-acting types of insulin, and you and your doctor will have to work together to decide on the right dose, timing, and type of insulin for you. You will need to test your blood sugar regularly at home if you’re taking insulin. Keep a blood sugar log so you can manage your treatment. Ask your doctor if you should check your sugar before or after meals. Write down the time, if it’s before or after you ate, what your blood sugar is, when you last had insulin, and what the dose was. Keep track of changes in your blood sugar before and after you exercise.
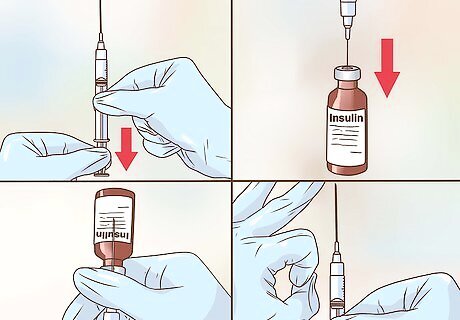
Take insulin injections if your doctor prescribes them. Insulin is often given as an injection using a syringe. Giving yourself insulin shots properly is important, so have your doctor demonstrate how to do it correctly. Ask any questions you have, for instance, “At what angle do I inject myself?” or, “Where are the best places to inject insulin?” Your doctor can probably refer you to a diabetes specialist to help you manage your insulin. Follow these general guidelines for insulin injections: Keep your unopened insulin in the refrigerator. Use a new needle for every injection and do not ever share needles. Rotate your injection site (that is, avoid always injecting yourself in the same place on your body, and change to a new location frequently). Do not use expired or frozen (even if defrosted) insulin.

Use insulin pens for more comfortable injections. Managing diabetes may be easier, and more comfortable, if you use an insulin pen. These hand-held devices use smaller needles than syringes, have dials for more accurate dosing, and can be conveniently carried around. Have your doctor or diabetes nurse show you how to use your pen properly, and follow similar guidelines for rotating injection sites and properly storing your pen.
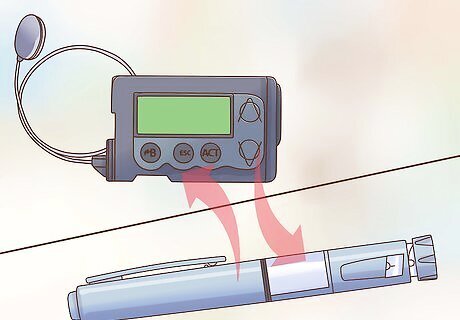
Get an insulin pump if you need to administer insulin continuously. Insulin pumps are small electronic devices that are attached to your body and deliver insulin through a small tube implanted into your side. It provides insulin continuously, which helps to avoid big spikes and drops in blood sugar. Discuss the risks and benefits of using a pump with your doctor – the convenience and comfort are often factors for users. Your doctor is more likely to recommend an insulin pump if you have type 1 diabetes rather than type 2. Even with a pump, you still have to monitor your blood sugar at home.

Talk to your doctor about medications to help your body make more insulin. Medications such as glyburide (DiaBeta, Glynase), glipizide (Glucotrol), and glimepiride (Amaryl) increase how much insulin your body makes. Ask your doctor if one of these medications may be right for you. Your doctor will prescribe one of these medications and you will work together to monitor your blood sugar. These medications are not used very frequently anymore. Talk to your doctor about the possible risks of using this type of medication, since they can cause problems with low blood sugar if you don’t take them with food. You might experience weight gain with sulfonylureas. In rare cases, your doctor may prescribe a different type of medication called a meglitinide. These work faster than sulfonylureas, but they don’t last as long.
Lifestyle Changes
Eat a healthy diet. Manage insulin resistance naturally by eating a diet low in sugar and fatty meats, and high in fruits, vegetables, and whole grains. Eat foods high in fiber like peas, beans, lentils, bran, oatmeal, and whole wheat. A dietitian can help you develop the best diet to manage your insulin resistance. Stay away from sweets, including sugary sodas. Skip processed snack foods like chips and other “junk-food” aisle products. Choose lean poultry and fish over red meat.
Limit how many carbs you eat during meals and snacks. Eating too many carbohydrates can put a high demand on the cells in your body that make and respond to insulin. Over time, this can make it harder and harder for your body to process insulin correctly. To prevent this from happening, keep tabs on how many carbs you eat by reading nutrition labels carefully and keeping a food diary. As a general rule, if you’re diabetic: Men should stick to no more than 60g of carbs per meal. If you’re a woman, limit your carbs per meal to 45g. Avoid eating more than 15g of carbs per snack between meals.
Exercise 5 days a week. Get aerobic exercise for at least 30 minutes a day, 5 days a week. Do anything that makes you sweat and raises your heart rate, like walking, biking, or swimming. Get creative—try dance, a sport, or an exercise class. Talk to your doctor before starting a new exercise regime, especially if you’re diabetic. Ask your doctor how exercise affects your blood sugar, and what you need to do to manage it.

Spend time in cool environments and eat healthy foods to increase your brown fat. Brown fat exists in small amounts in your body. In contrast to the white fat you think of when you think of weight gain, brown fat burns calories at a supercharged rate. It may be able to improve your body's sensitivity to insulin. Studies are still being done on brown fat, but the best ways to increase it seem to be: Cooling your body down for 2-3 hours a day by sitting in a cold room, taking cool baths or showers, or taking a long walk outside in a cool climate. Cold weather stimulates brown fat production. Exercising regularly in a cool environment, around 63–64 °F (17–18 °C). Get plenty of iron in your diet, and eat plant fats over animal fats (cook with olive oil instead of butter, for instance).












Comments
0 comment