views
X
Trustworthy Source
Centers for Disease Control and Prevention
Main public health institute for the US, run by the Dept. of Health and Human Services
Go to source
- Look out for flesh-colored lesions that are not filled with fluid and do not have dimples. These are all qualities of genital warts in men.
- Your doctor may prescribe medications like imiquimod, podofilox, or podophyllin. They may be applied in-office or at home, depending on the medication.[2]
- If your warts persist, consider surgical options like electrosurgery or cryotherapy. These are outpatient procedures with healing times of 1-3 weeks.[3]
Identifying Genital Warts
Examine your risk factors to see if an HPV infection is likely. Some behaviors and physiological traits put you at a higher risk for an HPV infection. Ask yourself the following questions to see if your risk of infection is elevated. Your doctor will most likely ask the same questions when you go in for testing: How many sexual partners do you have? The more partners, the more likely you can acquire the virus. Do you use condoms? This barrier helps reduce sexually transmitted diseases, including HPV. How old are you? Genital warts are most prevalent among adolescents, teenagers, and young adults. Do you have a severe infection or cancer, or are you taking drugs that damage your immune system? Infections such as HIV/AIDS reduce the body's ability to fight infections. Blood cancers such as leukemia alter our immune cells and cause them to be dysfunctional. Drugs such as steroids reduce our immune system over time. Did you notice any skin damage to your genitals? Breaks in your skins such as cuts give the virus an opportunity to enter your body. Do you have an uncircumcised penis? Men who have not had the foreskin of their penis removed are more likely to acquire HPV and pass it along to their partners. Do you smoke? Tobacco use increases your risk of infection from any type of HPV. The correlation is strongest for men smoking 10 or more cigarettes a day.
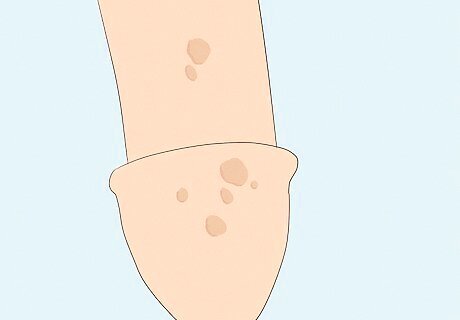
Look for flesh-colored lesions and other symptoms of HPV genital warts. It’s possible to confuse warts for other conditions that cause genital bumps or sores, like herpes or syphilis. Schedule an appointment with your doctor for a fast and proper diagnosis. In the meantime, look for the following characteristics of HPV to help you distinguish genital warts from other conditions at home: HPV warts are flesh-colored lesions and may be flat or raised. Redder, fluid-filled blisters are more likely genital herpes. HPV warts are not fluid-filled and do not burst open. Genital herpes blisters are painful and can open into a sore, spilling fluid before healing. An ulcer (open skin lesion) on your penis can also signify the first stage of syphilis. Lesions caused by syphilis are usually painless. HPV warts are not usually painful.Though not always painless, pain and itchiness are more associated with herpes than genital warts. HPV warts are not dimpled. A dimple on the top of the wart can indicate a viral infection known as mulluscum contagiosum. Mulluscum can be a sign of HIV infection as well. Other symptoms—including a red rash on the palms and soles, white patches in the mouth and genitals, fever, hair loss, and sore throat—in addition to genital warts may be secondary stage syphilis. Multiple small bumps around the base or tip of the penis that are either flesh colored, red, yellow, pink, or translucent could be a condition known as pearly penile papules and are completely harmless. This is considered a normal variant of penile skin and is not contagious.
See your doctor for an official diagnosis. Ultimately, a visit to your doctor is the best way to identify potential HPV warts. They will perform a physical examination as there is currently no test to detect HPV in men. Your doctor will also determine the best treatment options. HPV genital warts may clear up on their own, and about 70% of flare ups go away within 1 year. Sometimes, a doctor will not recommend treatment right away to see if the warts regress or if you develop more bothersome symptoms. In that case, observe the warts for: Increase in size Increase in number More in new places on your body Potential syphilis symptoms including itchiness, pain, bleeding from the warts, hair loss, fever, white patches on the mouth or genital area, a sore throat, or an ulcer on the penis. Syphilis can eventually lead to neurological problems over time if left untreated. Possible penile cancer symptoms including fatigue, weight loss, blood from your penis, lumps on your penis, a velvety rash, hardened penile skin, or smelly discharge. Visit a doctor as soon as possible if you notice these symptoms. HPV is responsible for approximately 63% of penile cancer in the USA. The median age of diagnosis is 68 years old but can be as early as your 30s.
Treating Genital Warts with Medication
See your doctor for safe treatment recommendations. Your doctor will perform a routine visual examination of the warts and the rest of your body looking for any additional warts. The doctor may apply a small solution of trichloroacetic acid to the area, which will whiten the warts to make them more visible and which can be used as a treatment to remove the warts. Talk to your doctor for more recommended treatment options. Treatments are based on many factors, including size and number of the warts, the area affected, previous treatments administered, and whether the outbreak is recurrent or not. Remember that there is no cure for the virus, only the warts themselves. Avoid over-the-counter treatments for the genital area. The genital skin is very sensitive and applying chemicals without proper knowledge and training can lead to irritation or damage.

Inquire about immune response modifiers. These medications will boost immune proteins in your body to help it get rid of the warts. These medications are available in various types, including: Imiquimod: Your doctor will apply a 5% imiquimod cream to the area using protective gloves and a pad, and prescribe a prescription for the cream afterward. At home, apply the cream before bed using disposable gloves or pads. After waking up in the morning (6-10 hours after applying treatment), wash the area with soap and water to remove it. Apply 3 times per week for the next 16 weeks. Interferon alphas: At the base of each wart, your doctor will inject 3 million international units (IU) of interferon. You will repeat this process with the doctor 3 times per week for the next 3 weeks. For bigger warts, multiple injections may be done. The warts should disappear after 4-8 weeks. If the warts remain after 12-16 weeks, your doctor may suggest a second treatment course.
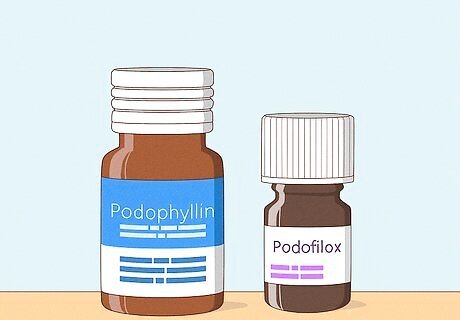
Ask about cytotoxic drug options. These drugs can destroy the warts and prevent the spread of them. However, they can also damage normal skin areas. If spilled or accidentally applied to an unaffected area, immediately remove the drug on the area(s) with water and soap. Side effects can include pain, irritation, itchiness, and redness. Options include: Podofilox: This is the preferred treatment for lesions less than 10 cm². To ensure correct usage (0.5 mL or 0.5g), your doctor will show you how much and how to apply the medication. Apply to the area using a cotton swab if liquid or using a finger if gel. Repeat twice daily for 3 consecutive days, followed by 4 days of no treatment. Repeat this process for up to 4 weeks. Trichloroacetic acid (TCA) or bichloracetic acid (BCA): These are both physician-applied treatments. Your doctor will apply the acid to the warts on a cotton ball. Your doctor may advise weekly treatment for up to 4-6 weeks. This is one of the most common treatments. Podophyllin: This is a physician-applied medication for warts less than 10 cm². Your physician will apply to the affected area sparingly. Your doctor will advise you to air dry the affected area to prevent it coming in contact with your clothes. Initial treatment should be left on for 30-40 min. Subsequent treatments can be from 1-4 hours, after which you’ll remove the podophyllin with soap and water. This treatment can be applied weekly for up to 6 weeks. This drug must not be used during pregnancy or possible pregnancy, so limit sexual exposure to a female partner during treatment. 5-Fluorouracil: Your physician may apply the first dose or provide a prescription. Using a cotton swab, apply it to the affected area 1-3 times per week. Use sparingly. Let the cream air dry to prevent contamination of your clothes. After 3-10 hours (specified with your prescriptions), wash the area with soap and water to remove it. Sinecatechins: Your doctor may prescribe this green tea extract. Use your finger to apply a small layer of 15% ointment to the affected area sparingly. Repeat 3 times daily with your finger for up to 16 weeks or until the warts have disappeared. Do not wash off and avoid sexual contact.
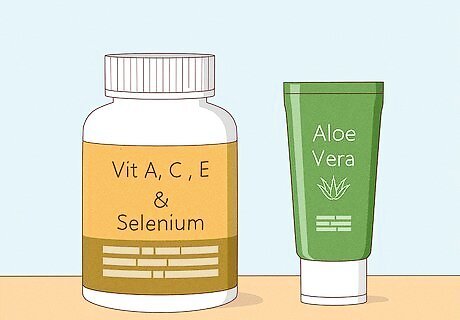
Look into home remedies that boost your immune system. There are a number of home remedies targeted for wart removal, though clinical studies are lacking. The concept of these treatments is to correct any nutritional deficiencies, which in turn helps your immune system fight off the warts. In addition, many of these treatments contain antioxidants that can fight infections. Always discuss new or home treatments with a naturopathic physician or your primary healthcare provider. Try soothing warts with plant-based botanical creams like aloe vera, burdock, or echinacea. Consider supplements for vitamins A, C, and E, as well as the minerals selenium and zinc. Stay on top of your hygiene to keep infected areas clean and prevent spreading the virus. Shower and clean your genitals regularly and avoid sharing towels (always wash them after use).
Considering Surgical Options
Consult your doctor about surgical options if medication is ineffective. Your doctor may suggest surgical procedures when large numbers of warts are present or a large area is affected. Your doctor may also recommend one of these options if you’ve had several recurrences of HPV warts. The typical cost for a wart removal procedure, like cryotherapy, laser treatment, or surgical excision, is typically about $200 to $300 per procedure.
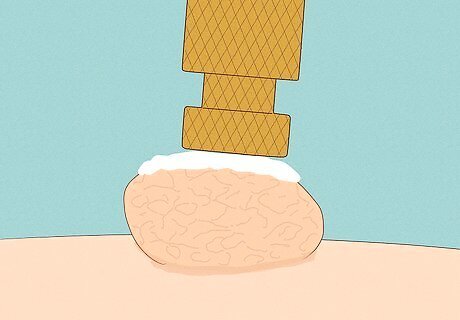
Ask about cryosurgery. An application of liquid nitrogen solution freezes the water found inside the warts, causing destruction of the cells that make up the warts. The provider will clean the area of the warts with an alcohol swab. An applicator tip containing liquid nitrogen will be applied to each wart until they're frozen. An additional 30 seconds of freezing will be done until the skin turns white, followed by a thawing period where the white area disappears. If you’re sensitive to pain, ask about local anesthesia to numb the treatment area. After 2-4 treatments within 6-12 weeks, 75-80% of patients experience a complete clearing of warts. Store kits are available for this procedure, but healthcare professionals recommend having a doctor administer it.
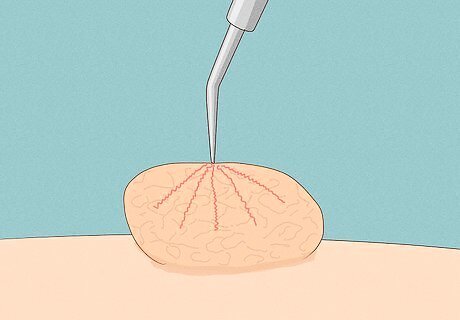
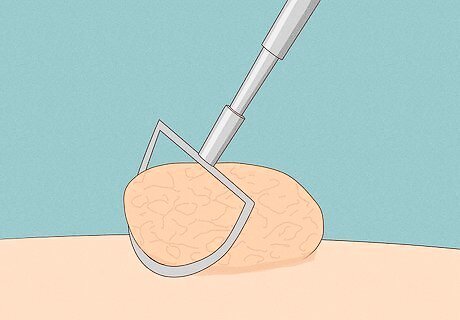
Inquire about a loop electrosurgical excision procedure (LEEP). Also called electrosurgery, this procedure uses a high-frequency electrical current needle to cut the warts from your skin. Your doctor will apply a local anesthetic to the area first and you’ll be able to leave the office the same day. Most people can return to normal activities after 1-3 days, but sex should be avoided until the procedure site is fully healed (typically within 1-3 weeks). Following the procedure your doctor may prescribe pain medication if needed. Electrosurgery has been found effective for a small number of lesions on the shaft of the penis. Side effects are rare but may include scarring on the penis or possible problems with urination or erection. Post-procedure infection is rare and can be treated with antibiotics.
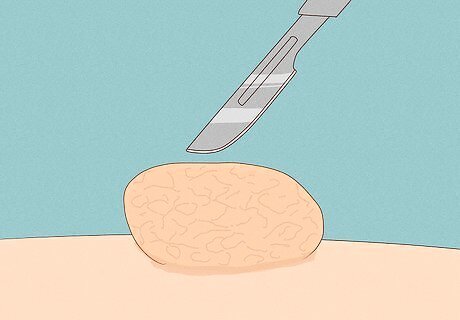
Determine if surgical excision is the right option. For this option, your doctor will cut the wart out with a scalpel. For a minimal number of small warts, your doctor will inject 1% lidocaine anesthesia to numb the area. However, general anesthesia may be used for more extensive cases. Your doctor may suture the two sides of healthy skin back together depending on the size of the excised wart. Removing warts may leave scars, and it’s possible for warts to return. Healing typically takes 2-4 weeks, but most people can return to normal activities in 1-3 days.
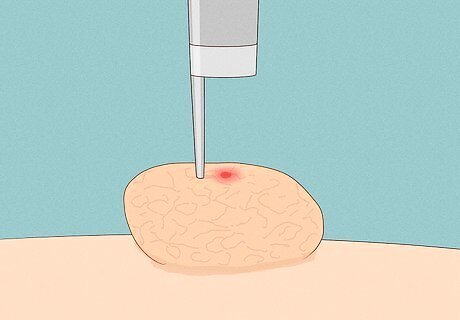
Ask your doctor about laser surgery. This method uses a carbon dioxide laser to evaporate the wart and is especially helpful in recurrent cases. This is an outpatient procedure done at your doctor's office (usually a dermatologist). Your doctor will administer a general or regional anesthetic to prevent any pain or discomfort from the laser. Your doctor will likely prescribe pain medication for after the procedure since most patients report significant discomfort after the surgery. It is extremely important not to move while the laser is targeted on your skin as this may lead to damage to normal tissue. Full healing may take 2-4 weeks, and sex should be avoided for at least 1-3 weeks until the procedure site is healed and all soreness is gone.


















Comments
0 comment