
views
X
Trustworthy Source
Cleveland Clinic
Educational website from one of the world's leading hospitals
Go to source
It’s often asymptomatic, especially in men, which makes it difficult to trace and detect without regular STI testing. For those men that show symptoms, it’s important to recognize them quickly and seek treatment right away to prevent spreading it to sexual partners or contracting secondary infections like epididymitis. In this article, we’ll show you the most common genital symptoms and other bodily signs of chlamydia, plus walk you through the (thankfully simple) diagnosis and treatment process. Remember, awareness about your sexual health is the best way to prevent STIs and enjoy yourself responsibly!
- Look for common chlamydia symptoms like discharge from the penis, burning urination, irritation around the opening of the penis, or swollen or painful testicles.
- Watch out for other bodily symptoms like an inflamed prostate, burning or red eyes, rectal pain or bleeding, or swollen lymph nodes in your groin.
- Visit your doctor if you were exposed to or contracted chlamydia to get tested. Take your antibiotics as prescribed (infections usually clear up in 1-2 weeks).
- Get an STI test at least once a year. Prevent chlamydia by wearing condoms during sex and being open with your partners about each others’ sexual health.
Common Genital Symptoms

Burning during urination (dysuria) Notice if you experience any pain, burning sensations, or discomfort along your urethra or near the opening of the penis while you’re urinating. This indicates the infection is in your urethra and is one of the most common chlamydia symptoms in men.
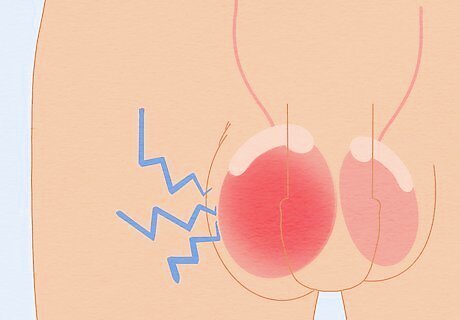
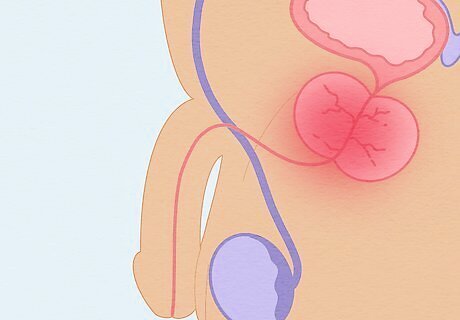
Pain or swelling in the testicles or scrotum Watch out for pain, inflammation, or redness in or around one or both testicles. The swelling and tenderness may spread to the scrotum as well. Testicular or scrotal inflammation may be an early sign of epididymitis caused by chlamydia (chlamydial epididymitis).
Testicular pain, a red or inflamed scrotum, fever, or bloody urination Look for epididymitis symptoms if you suspect you have chlamydia, especially if it has gone untreated. Epididymitis most commonly occurs when severe or untreated chlamydia spreads from the urethra to the epididymis and causes another infection. See a doctor immediately if you’re experiencing any epididymitis symptoms or pain and swelling in your testicles or scrotum. Epididymitis is an infection of the epididymis (the tube connecting the testes to the vas deferens) caused by bacteria from STIs like chlamydia.

Discharge from the penis Look for mucus-like or clear, watery discharge coming from the tip of the penis. Not all men will experience discharge, but it is one of the most common signs of chlamydia in men who show symptoms. The discharge may not “flow” out of the penis on its own and might only be visible if it’s squeezed out. Discharge from chlamydia is usually less profuse and thick than from gonorrhea. Recognizing gonorrhea symptoms can be tricky since they’re similar to those of chlamydia.
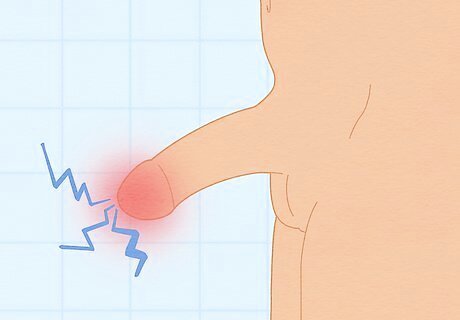
Itching or burning around the opening of the penis Take note if the discomfort you feel during urination continues when you’re done. This could indicate you’ve developed an infection of the urethra, known as urethritis, from your chlamydia. Urethritis might also be called non-gonococcal urethritis, which means it was caused by something other than gonorrhea.
Other Bodily Symptoms
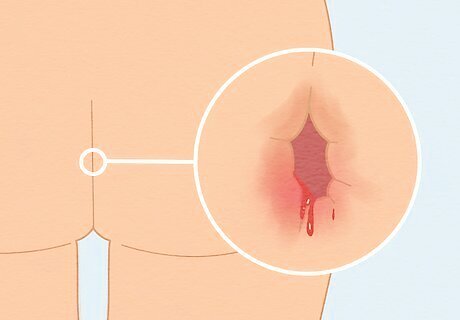
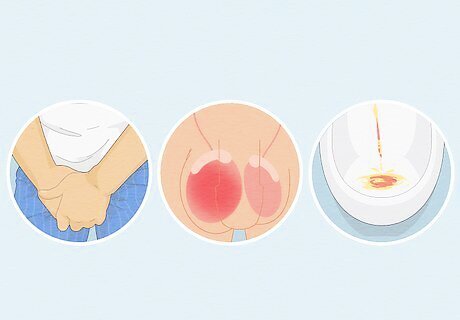
Rectal pain, bleeding, or discharge If you’ve engaged in anal sex and suspect you may have an STI like chlamydia, look out for pain or discomfort, bleeding, or a mucus-like discharge coming from your bottom. See your doctor immediately if you’re experiencing any of these symptoms.
Prostate inflammation Notice if you’re experiencing pain during urination or ejaculation, incontinence, difficulty urinating, or pelvic pain. These could be signs of chronic prostatitis (long-term inflammation of the prostate gland possibly caused by chlamydia and other STIs). Prostate problems are more likely if the chlamydia infection is rectal rather than in the urethra.
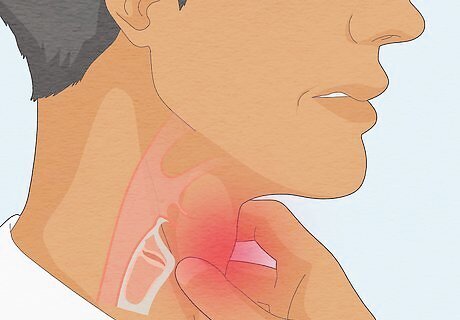
Sore throat If you’ve had oral sex recently, watch out for a sore throat or pain while swallowing. It’s possible for the Chlamydia trachomatis bacteria to spread from an infected person’s genitals to their partner’s mouth or throat during oral sex, but this is less common than during vaginal or anal sex. There aren’t typically other symptoms besides a sore throat if you’ve contracted chlamydia orally.
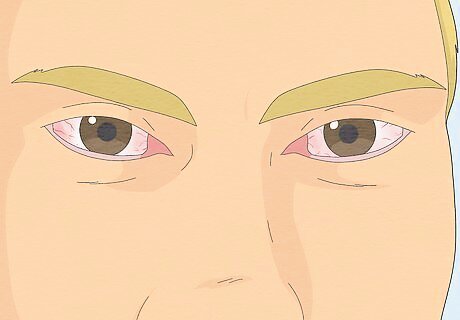
Redness or pain in your eyes Look for symptoms similar to conjunctivitis (pink eye) like pain or irritation, dryness, redness, or discharge that crusts up. A chlamydial eye infection is only likely if bodily fluids containing chlamydia bacteria got in your eye during intimacy.
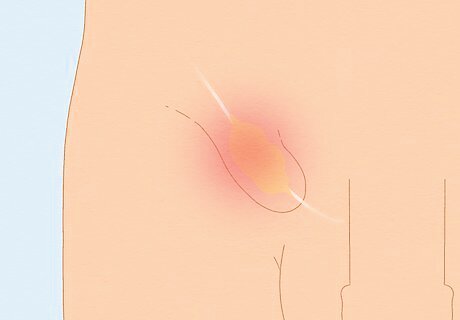
Painful, swollen lymph nodes in your groin Examine your groin for swollen, painful lumps or a painless ulcer near your penis, mouth, or anus. Some strains of chlamydia cause a separate infection called lymphogranuloma venereum (LGV), an STI that inflames the lymph nodes near where the bacteria entered the body. LGV spreads the same way as chlamydia, but requires a more aggressive antibiotic treatment to cure than most strains of chlamydia.
Swollen, stiff, or painful joints Assess your knees, ankles, and feet for pain, swelling, redness, or stiffness (this can occur in other joints too, but is more common in the lower body). About 1% of men with urethritis caused by chlamydia get reactive arthritis, an immune reaction that causes arthritis-like pain throughout the body. Some men with reactive arthritis may feel lower back pain, pain where tendons and ligaments connect to bone (enthesitis), and swollen fingers (dactylitis).
Diagnosis & Treatment
Monitor your sexual health if you’re at risk of contracting chlamydia. Chlamydia can be caught through vaginal, anal, or oral sex, or sex that involves sharing toys. If you’ve engaged in these activities with an infected person, a person with an unknown STI status, or without a condom, there is a chance you could get chlamydia. You’re more likely to be diagnosed with chlamydia if: You’ve been diagnosed with other STIs You’re a teen or young adult aged 15 to 24 (this demographic makes up about half of US cases per year) You’re a man who has sex with men (MSM) You’re Black and non-Hispanic (High transmission rates among specific demographics, like non-Hispanic Black people or MSM, are largely due to networks and access to preventative care rather than sexual behavior)
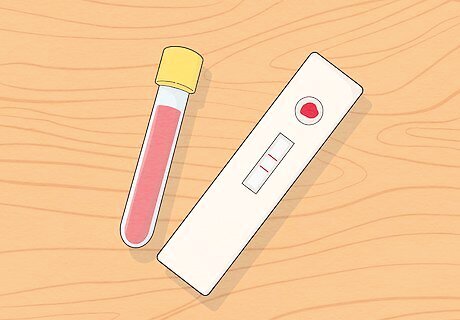
Get tested for STIs regularly, even if you have no symptoms. Get a full STI screening, including for chlamydia, at least once a year (or more often if you regularly have multiple sexual partners). Also test after you have unprotected sex, have sex with a new partner, or experience any chlamydia-related symptoms after sex. Regular testing is the only way to know for sure whether you have chlamydia or not since it’s asymptomatic most of the time. Chlamydia can be asymptomatic for both men and women, making it easy to spread without knowing. It’s sometimes called the “silent infection.” Men who present chlamydia symptoms can have the infection for weeks before any noticeable signs appear.
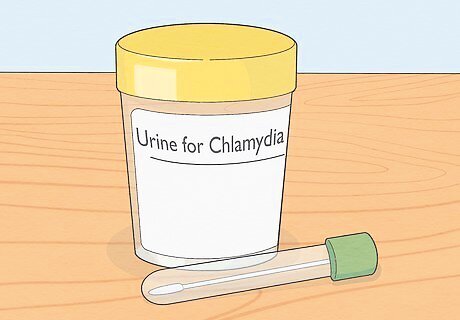
Visit your doctor if you notice any symptoms of chlamydia. Tell them about your symptoms and your recent sexual activity, especially if you’ve had unprotected sex with someone new. Get tested at each site where you have sex (mouth and throat, penis, and/or anus) so you don’t miss locations where the bacteria might spread. Lab tests for chlamydia can include a urine test and/or swabs taken from your urethra, throat, or rectum. The results can take up to a week to come back. Your doctor may prescribe you antibiotics before the results are back as a precaution. If you don’t have a doctor or insurance, visit local clinics or a sexual health agency like Planned Parenthood for free testing or sliding scale payment. If you suspect you have chlamydia, tell all of your recent sexual partners to get tested as well.
Begin your antibiotic treatment right away. Follow your doctor’s instructions and take your antibiotics as prescribed—some treatments involve one large dose, while others require multiple pills taken over 7-10 days or more. Your treatment may also include antibiotics for gonorrhea, since the symptoms are very similar and it’s common to have both STIs at once. When you take your medication correctly, most chlamydia infections clear up within a week or two. Antibiotics for chlamydia are usually oral medications like azithromycin or doxycycline.

Wait at least 7 days after you begin treatment to have sex again. Stay away from sex until your symptoms have cleared up completely. If you took one large dose of antibiotics, this usually happens after 7 days. If you have a longer prescription, wait until you’ve finished taking every prescribed dose and all of your symptoms are gone.

Prevent a repeat infection by wearing condoms during sex. Use a latex condom during all sexual activity to greatly reduce (but not 100% eliminate) your risk of getting chlamydia. Make sure it fits snuggly over your penis and check it throughout sex to make sure it hasn’t broken. If you or your partner is allergic to latex, use polyurethane condoms instead. To prevent oral transmission, use a dental dam during oral sex to keep chlamydia bacteria from entering the throat from the vagina or anus. Be open with your sexual partners about your STI status, and ask them about theirs. Good communication about sexual health can prevent transmission. The only surefire way to prevent chlamydia is to abstain from all vaginal, anal, or oral sex.













Comments
0 comment