views
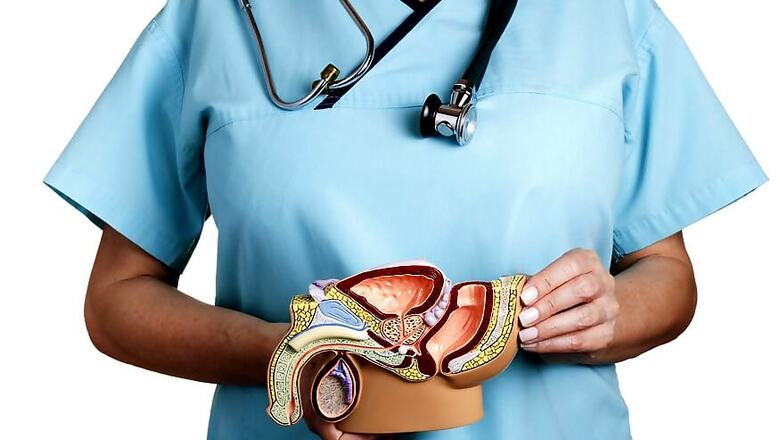
Men with low or intermediate-risk prostate cancer can safely undergo higher doses of radiation over a significantly shorter period of time and still have the same, successful outcomes as from a much longer course of treatment, according to researchers including one of Indian-origin.
The study showed that this type of radiation - stereotactic body radiotherapy - is a form of external beam radiation therapy, which reduces the duration of treatment from 45 days to four to five days with no evidence of causing worse toxicity in the long run.
"Most men with low or intermediate-risk prostate cancer undergo conventional radiation, which requires them to come in daily for treatment and takes an average of nine weeks to complete," said lead author Amar Kishan, Assistant Professor at University of California, Los Angeles, in the US.
"With the improvements being made to modern technology, we have found that using stereotactic body radiotherapy, which has a higher dose of radiation, can safely and effectively be done in a much shorter timeframe without additional toxicity or compromising any chance of a cure," said Kishan.
For the study, the team included 2,142 men with low or intermediate-risk prostate cancer who were treated with stereotactic body radiotherapy. They were followed for a median of 6.9 years.
Nearly, 53 per cent men had low-risk disease, 32 per cent had less aggressive intermediate-risk disease and 12 per cent had a more aggressive form of intermediate-risk disease.
In addition, the recurrence rate for men with low-risk disease was 4.5 per cent, 8.6 per cent for the less aggressive intermediate-risk, and 14.9 per cent for the more aggressive intermediate-risk group, findings published in the journal JAMA Network Open showed.
Overall, the recurrence rate for intermediate-risk disease was 10.2 per cent.
These are essentially identical to rates following more conventional forms of radiation, which are about 4-5 per cent for low-risk disease and 10 per cent to 15 per cent for intermediate-risk disease.
This method is both safe and effective and could be a viable treatment option for men with low and intermediate-risk of prostate cancer, the study suggested.


















Comments
0 comment