views
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
Research suggests that pneumonia may cause symptoms like cough, shortness of breath, chest pain when you breathe or cough, fever, and chills, which may be severe. Since pneumonia may be caused by a bacteria, virus, fungi, or inhalant, the right treatment for you will vary.[2]
X
Trustworthy Source
MedlinePlus
Collection of medical information sourced from the US National Library of Medicine
Go to source
Visit your doctor to get a proper diagnosis so you can get prompt medical care.
Treating Pneumonia
Take care of mild cases. If you have a mild case of pneumonia like walking pneumonia, you will be treated as an outpatient. If the patient is a child, she may be admitted to the hospital if the doctor thinks it may get worse. Your doctor will start you on an antibiotic regimen. Your doctor will also suggest rest and increased sleep in order to get better as quickly as possible. Even in mild cases, you should not go to school or work until your doctor says you can. Total recovery is generally seven to 10 days. Some types of pneumonia are highly contagious, while others are only passed to others under optimal conditions. When you are diagnosed, ask your doctor about how contagious your particular pneumonia is, and for how long you will be considered contagious. You should see a significant improvement in your symptoms within 48 hours of treatment. This means you should no longer have a fever and have an overall increase in strength. There is no need for special care when cleaning up after a patient with pneumonia. The germs that cause it are not viable on inanimate objects for any substantial time frame and will be removed with normal washing.
Deal with moderate cases. Moderate cases of pneumonia are those with significant respiratory compromise and require supplemental oxygen to keep their oxygen saturation up. These patients will also have fever and overall sickly appearance. If this is how your pneumonia manifests, you will likely be admitted to inpatient wards to receive intravenous antibiotics. The kind of antibiotics you get will not change, they will just be in IV form in order to get the drugs into your system faster. You will be changed to oral antibiotics as your fever breaks and you become responsive to therapy. This typically takes no more than 48 hours. The treatment from here follows the same for mild cases, because the case has transitioned from moderate to mild.

Seek help for severe cases. Severe cases of pneumonia are those with patients who are going through respiratory failure. This requires intubation and mechanical ventilation. It may also require being admitted to the intensive care unit. Like with moderate cases, IV antibiotics are required. These cases often require vasopressor support with pressors (medications which raise your blood pressure) to counter the effects of septic shock. While in the hospital, you will need supportive care to improve your general health while the medications do their work. Once you improve, you will follow the care for moderate and then mild cases as you get better. The length of your hospital stay will depend on the severity of the damage to your lungs and how bad your case of pneumonia was. Your doctor may utilize bilevel positive airway pressure (BiPAP) in select patients to prevent intubation and traditional mechanical ventilation. BiPAP is a non-invasive way to deliver pressurized air to a patient, often used to treat sleep apnea.
Take the right antibiotics. There are a few different antibiotics that you can take if you get pneumonia. Your doctor will determine which kind of pathogen caused your pneumonia, which will then determine which medicine you take. For the most common forms of pneumonia, antibiotics such as zithromax or doxycycline are combined with amoxicillin, augmentin, ampicillin, cefaclor, or cefotaxime. The dosage will depend on the age and severity of your case, as well as your allergies and the culture results. You doctor may prescribe the less common but effective single antibiotic therapy route, which is a respiratory quinolone such as Levaquin or Avelox for adults. Quinolones not indicated for pediatric populations. In moderate cases and mild cases on the verge of hospitalization, your doctor may give you a rocephin IV followed with the oral regimen. In all these cases, your doctor will follow up within a few days to see how your symptoms are progressing.

Treat hospital-acquired pneumonia (HAP). Patients that get HAP are already dealing with health issues. This makes their treatment a little different than community-acquired pneumonia (CAP), though these methods may be used in rare and severe cases of CAP. HAP can be caused by many different types of pathogens, so your doctor will determine which kind you have and then administer the antibiotics according to the pathogen infecting your. The common treatments are: For Klebsiella and E Coli, IV antibiotics such as quinolone, ceftazidime, or ceftriaxone For Pseudomonas, IV antibiotics and imipenem, piperacillin, or cefepime For Staph Aureus or MRSA, IV antibiotics such as vancomycin For fungal pneumonias, IV antibiotics such as Amphotericin B or Diflucan IV For vancomycin resistant enterococcus: IV antibiotics of Ceftaroline
Preventing Pneumonia
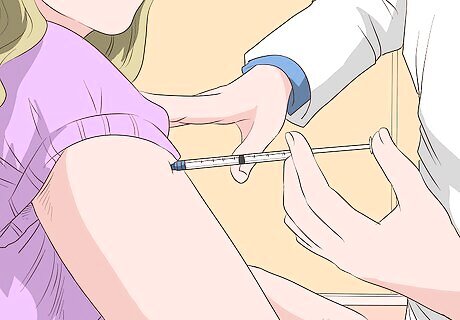
Take the flu shot. Pneumonia can be caused when influenza is contracted and becomes advanced. Because of this, it is recommended that you get the flu shot every year. Since this helps fight against the flu, it will help fight against pneumonia as well. The flu shot can be taken by anyone over the age of six months. There is a special vaccine that can be taken by children younger than two and also one for those two to five years old who are at increased risk of pneumonia. Children who go to communal day care should also get the vaccine. There is also a vaccine for those without spleens, over the age of 65, with lung disease such as asthma and COPD, and with sickle cell anemia.

Wash your hands often. If you want to avoid getting pneumonia, you need to avoid coming into contact with the viruses and germs that cause it. You can do this through proper hand washing. If you are in public or around someone you know is sick, you should wash your hands as much as possible. Also avoid putting your unclean hands near your face in order to prevent the spread of unwashed germs from your hands to your system. To wash your hands properly, you need to: Turn on the faucet and wet your hands. Apply soap to your hands and scrub every part of your finger. This includes under the nails, on the backs of your hands, and between your fingers. Keep rubbing your hands for at least 20 seconds, which is how long it takes to sing the "Happy Birthday" song all the way through twice. Rinse your hands in the water to rinse off the soap. Make sure the water is warm to help remove the soap and germs. Dry them off with a clean towel.
Take care of yourself. A great way to prevent contracting pneumonia is to be in the best overall health you can be. This means you need to stay in shape physically and mentally. Try to exercise every day, eat a healthy and well-balanced diet, and get enough sleep. These things all benefit your health and will keep your immune system in the best shape it can be, which will help you stay as healthy as possible. Many people think they can skimp off sleep and still be healthy. Studies have been done that link the wellbeing of your immune system to the amount of sleep you get each night. The more high-quality sleep, which is uninterrupted sleep in a sleep-conducive environment, you get a night, the healthier your immune system will be.

Try vitamins and minerals. There are some supplements that you can take to boost your overall immune health. One of the best to help pneumonia is Vitamin C. Take between 1000 to 2000 mg every day. You can get this from citrus fruit, citrus juice, broccoli, watermelon, cantaloupe, and many other fruits and vegetables. Zinc is helpful if you feel like you are getting a cold, which can turn into pneumonia. At the first sign of symptoms, take 150 mg of zinc three times a day.
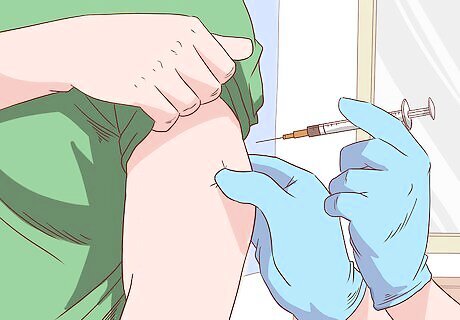
Get a pneumonia vaccine if you have a weak immune system. While getting a flu shot is useful for nearly everyone, pneumonia vaccines are only really necessary for some. If you're a healthy adult between the ages of 18 and 64, you probably don't need to worry about getting vaccinated. However, consider getting vaccinated if you are over 65, have a disease that makes your immune system weak, smoke or drink heavily, or are recovering from a major illness, injury, or surgery. The two types of pneumonia vaccines are: The pneumococcal conjugate vaccine (PCV13 or Prevnar 13) which protects against 13 types of pneumococcal bacteria and The pneumococcal polysaccharide vaccine (PPSV23 or Pneumovax) which protects against 23. Getting a pneumonia vaccine doesn't guarantee that you won't get pneumonia, but it drastically lowers your chances. If you do get pneumonia after taking a pneumonia vaccine, it'll most likely be a mild case.
Understanding Community-Acquired Pneumonia
Learn the types. Pneumonia is divided into two broad types that are caused by different things and are treated differently — community-acquired pneumonias (CAP) and hospital-acquired pneumonia (HAP), which will be discussed later. CAP consists pneumonia caused by typical bacteria, atypical bacteria, and respiratory viruses. CAP is the kind of pneumonia most people contract in their daily lives. CAP is more dangerous in the elderly, the very young, and those with a compromised immune system, such as those with diabetes, with HIV, on chemotherapy, and taking steroid medications. CAP can range from a mild case treated at home to a case with acute respiratory failure and death.

Recognize the symptoms of pneumonia. The symptoms of pneumonia can vary from mild to severe, depending on the type of germ causing the pneumonia and how badly the patient is infected. If you notice any of these symptoms, see your doctor immediately to get treated. The longer you wait, the worse you can get. Symptoms of CAP include: A productive cough Mucus with a thick texture, which may be green, yellow, or red tinged Severe chest pain when a deep breath is taken Fever greater than 100.4°F (38°C), but often 101 to 102°F (38.3 to 38.9°C) Chills or involuntary shaking Shortness of breath, which can be mild to severe Rapid breathing, which is more common in child cases Drop in oxygen saturation in the lungs

Diagnose CAP. When you see your doctor, they will check for all the common symptoms. In addition to this, he or she will also take a chest radiograph, which will show how your lungs are affected. If your doctor see an area of white patchy consolidation on a lobe of the lung, which should usually be black, you likely have pneumonia. There may be a parapneumonic effusion, or collection of fluid, adjacent to the area of infection. Blood tests are not typically needed in mild cases of pneumonia. However, if your case is more advanced, your doctor may take labs such as a complete blood count, a basic metabolic panel, a mucus specimen, and cultures.

Seek immediate medical attention. There are certain circumstances in which you may need to see immediate medical care. Even if you have been treated, you should seek immediate medical help if your symptoms get worse. Get to a doctor or emergency room as soon as possible if: You become confused about time, people or places Your nausea and vomiting prevent you from keeping down oral antibiotics Your blood pressure drops Your breathing is rapid You need breathing assistance Your temperature is higher than 102°F (38.9°C) Your temperature is below normal
Understanding Hospital-Acquired Pneumonia

Know about hospital-acquired pneumonia (HAP). HAP occurs in patients who contract pneumonia while hospitalized. HAP refers to pneumonia that patients acquire while in the hospital. This strain is typically very severe and is accompanied by high death rates. It accounts for up to 2% of all rehospitalizations. It happens to all kinds of hospital patients, from those who are getting surgery to those who had a fall to those already with a serious infection. Hospital acquired pneumonia can lead to sepsis and multi-organ failure, and death. The symptoms of hospital acquired pneumonia are the same, since they are both types of the same disease.

Recognize the risks of hospital acquired pneumonia. Community acquired pneumonia is spread through the transmission of common pathogens. Hospital acquired pneumonia, however, is spread within a hospital. There are some patients that are more at risk than others based on their condition, though anyone in a hospital can contract HAP. These risk factors include: Being in the ICU Being on a mechanical ventilation for 48 hours or more Staying at the hospital or ICU for an extended time Those with severe issues with their underlying issues when they were originally hospitalized Those with heart failure, renal failure, liver failure, COPD, and diabetes

Learn the causes of hospital acquired pneumonia. Hospital acquired pneumonia can occur through complications after surgery, such as a post surgery collapsed lung or from not taking enough deep breaths due to pain. It can also occur due to poor hygiene from the medical staff at the hospital, especially while caring for patients with central lines, those one ventilator care, and those having a breathing tube placed or replaced.

Avoid hospital-acquired pneumonia. HAP can be avoided through excellent hygiene amongst healthcare providers, meticulous ventilator care, and post-operative use of incentive spirometers, which are devices that encourage deep breathing among post surgical patients. It can also be avoided if a person gets out of bed faster after surgery and if any intubations are removed as soon as possible.



















Comments
0 comment