views
X
Trustworthy Source
US Office on Women's Health
U.S. government agency providing resources for women's health
Go to source
Also known as vaginal candidiasis, yeast infections form from an overgrowth of a bacteria called Candida and rarely go away on their own, but thankfully, there are many ways to treat it. We’ve put together a guide of everything you need to know about taking care of yeast infections, from treating them with over-the-counter medications to preventing them with a tall glass of cranberry juice. So, take a deep breath and get ready to show Candida who’s boss!
- Try over-the-counter topical treatments like Monistat and Vagistat-1 if you have minor or mild symptoms.
- Talk to your doctor about taking a single-dose oral treatment like Diflucan to quickly ease mild yeast infection symptoms.
- Drink 6 to 19 oz (177 to 296 mL) of 100% cranberry juice a day and eat live culture yogurt to improve your vaginal bacterial health and prevent yeast infections.
Symptoms and Diagnosis
Abnormal discharge, pain, and itching could be signs of a yeast infection. Yeast infections make themselves known in a variety of ways. If something feels off down there, check for these symptoms, as experiencing one or more of them could mean you have a yeast infection: Itching, soreness, redness, and overall discomfort in the vaginal area. Pain or burning during urination or sex. Thick, white vaginal discharge that looks like cottage cheese.
Treatments
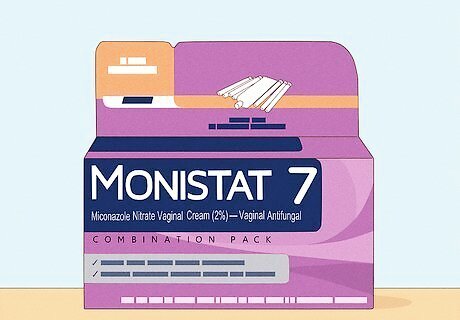
Use an over-the-counter topical treatment for minor to mild symptoms. Creams such as Monistat (miconazole nitrate) and Vagistat-1 (tioconazole) are some of the most popular treatments because readily available. Anti-fungal creams, ointments, and suppositories are applied on the vaginal area to eliminate yeast and extra bacteria. Follow the instructions on the back of the medication’s packaging, as they’ll tell you how often the treatment needs to be applied. If you can’t find these products or need financial support, your doctor can prescribe Mycelex (clotrimazole) and Gynezol or Femstat (butoconazole). There are over-the-counter oral treatments as well, such as AZO’s Yeast Plus Dual Relief tablets, but it’s always best to see a doctor before taking an oral treatment, especially if you take other medications.
Contact your primary care doctor if you’re experiencing new symptoms. If you’ve never had a yeast infection before or are experiencing severe or worsening symptoms (especially after trying other remedies), reach out to your doctor or gynecologist. They’ll be able to perform an exam to give you a proper diagnosis and an individualized treatment plan. A brief vaginal exam will most likely be performed, which simply involves the doctor swabbing a sample of your vaginal discharge to diagnose it. Mild to severe yeast infections won’t go away on their own, so it’s important to contact your doctor if symptoms worsen or persist.
Take a prescribed oral treatment for mild symptoms. If your symptoms aren’t severe and you don’t have pelvic pain or a fever, your doctor may provide you with a single-dose tablet of anti-fungal medication such as Diflucan (also known as fluconazole). This medication is taken by mouth once and should provide relief within 12 to 24 hours. Diflucan is the most popular yeast infection oral medication, but it’s not safe to use while pregnant. If you think there’s a chance of pregnancy or you’re breastfeeding, tell your doctor immediately.
Causes
AntibioticsAntibiotics kill bad bacteria to help you get over an infection or illness, but they can also kill good bacteria in the process. For some women, taking a routine or prescribed antibiotic for several days can cause an overgrowth of yeast in the vaginal area as there isn’t enough bacteria to control it. If you’re taking antibiotics, ask your doctor about what you can do to minimize your risk of getting a yeast infection. Symptoms of a yeast infection may not present themselves until after you’ve finished your round of antibiotics.
Birth control pillsOne of the leading causes of yeast infections is hormonal imbalances or changes. Oral contraceptives or birth control pills (BCPs) alter your estrogen levels to regulate menstrual cycles and prevent pregnancy. Higher estrogen levels attract Candida and can increase your risk of infection. Not all birth control pills contain estrogen. If you’re susceptible to yeast infections, talk to your doctor about switching to an estrogen-free contraception or progestin-only BCP.
Underlying health conditionsYou may be more likely to get a yeast infection if you have an underlying medical condition, compromised immune system, or high blood sugar. Higher blood sugar levels can promote Candida growth, so stay on top of your levels to avoid infection, especially if you have diabetes. HIV attacks your immune system, weakening your body’s natural defenses. Talk to your doctor about how you can prevent yeast infections while treating HIV. If you have another chronic or autoimmune condition, be cautious when taking medications that compromise your immune system. Being aware and taking preventative actions can help you avoid future yeast infections. Take care of your general health, as obesity, stress, and poor sleeping habits can contribute to yeast infections.

PregnancyWhen you’re pregnant, your body goes through all types of changes, which can make your hormones a bit wacky. Yeast infections are common in the second trimester of pregnancy because of this. If you experience abnormal vaginal pain, discharge, or irritation, reach out to your doctor to put together a yeast infection treatment that’s safe for you and the baby. Doctors generally recommend vaginal creams and suppositories to treat yeast infections in pregnant women, as oral medications could cause complications.
Preventive Care
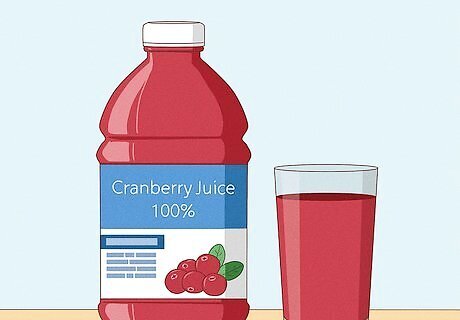
Drink 100% cranberry juice regularly to prevent yeast infections. Believe it or not, cranberries are one of the most powerful berries. They’re delicious, nutritious, and can help lower vaginal pH levels. Although this remedy isn’t completely proven to combat yeast infections, it won’t hurt to try drinking 6 to 10 oz (177 to 296 mL) of cranberry juice a day to see if it helps. Make sure your juice is 100% cranberry, not cranberry juice cocktail, as the formulated cocktail won’t give you the same health benefits. If you can’t find 100% cranberry juice in your area, try adding a cranberry supplement to your daily vitamins.
Eat yogurt with live cultures for an extra probiotic boost. Not only is yogurt delicious, but it’s also full of health benefits. Live culture yogurt is full of L. acidophilus, a bacteria that keeps Candida in check. Snacking on yogurt helps boost your good bacteria and control your vagina’s pH balance, so yeast infections are harder to get. Try swapping your morning cereal with a yogurt bowl or picking up a yogurt cup instead of a pudding as your evening snack. Now, yogurt won’t necessarily cure your yeast infection, but it can help prevent it from returning. Some women put plain, live culture yogurt on their vagina like a cream to ease yeast infection symptoms; however, doctors strongly advise against this as it could worsen symptoms.
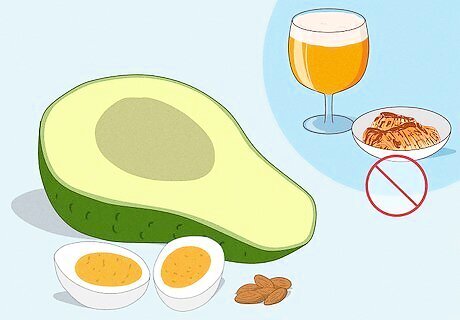
Try the Candida diet to reduce yeast growth. One way women have been easing yeast infection symptoms is by changing their diet. This treatment isn’t maintainable for everyone, especially long term, but it can provide short-term relief. When you feel like you have a yeast infection, eliminate white flour and rice, fermented foods and drinks, and simple sugar foods from your diet. Focus on eating more fats, proteins, and low-starch fruits and vegetables. Try to avoid wine, beer, cheese, kimchi, and sauerkraut. Snack on hard-boiled eggs, nuts, avocados, peaches, and cucumber.
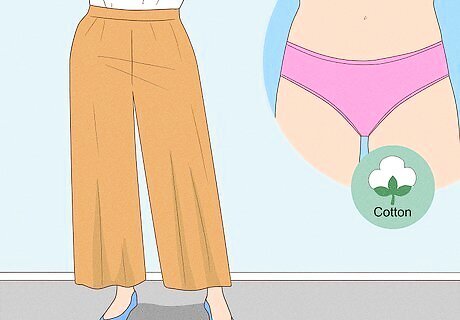
Wear cotton underwear and loose-fitting pants. Help your vagina “breathe” and stay cool throughout the day to eliminate moisture and bacteria growth. Yeast thrives in moist, warm environments, so making sure your clothes are dry and provide airflow can keep yeast infections from happening. Avoid silk and nylon underwear, as these materials trap moisture.
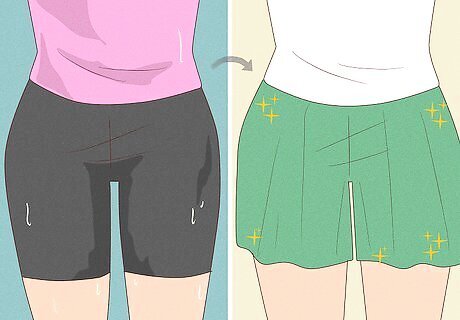
Change your clothes frequently, especially after getting wet or sweating. Yeast likes wet environments, and sitting in wet or damp clothing can cause it to fester, increasing your risk of infection. Make sure to change out of a wet bathing suit or tight, sweaty gym clothes as soon as possible.

Avoid douches and perfumed feminine products to protect your pH balance. Believe it or not, douching can actually do more harm to your vagina than good. Spraying water into your vagina to clean it out removes your healthy bacteria lining, leaving you more susceptible to infection. Along with this, the chemicals in scented pads, hygiene sprays, body washes, or powders can upset your vagina’s natural pH balance. Instead of douching, let your vagina wash itself—it knows what it’s doing. Use all natural feminine products to reduce your risk of infection.



















Comments
0 comment