
views
Using Diet and Lifestyle Modifications

Add soluble fiber to your diet. Diarrhea is a result of too much water in the colon. This happens when undigested, liquid food passes through the small intestine and colon too quickly, preventing the excess water from being absorbed into the bloodstream. Soluble fiber absorbs excess fluid in the bowel like a sponge, firming up loose stool. Try to include at least one portion of a fiber-rich food with every major meal. Foods rich in soluble fiber include: apples, beans, berries, figs, kiwi, legumes, mangoes, oats, peaches, peas, plums and sweet potatoes. Fruit should be eaten without the skin. Be aware that the use of fiber to treat IBS is somewhat controversial and may require some trial and error experimentation to see if it helps alleviate your diarrhea.

Avoid caffeine. Caffeine stimulates the gastrointestinal system, leading to strong contractions and more bowel movements. Additionally, caffeine has a diuretic effect, which may worsen dehydration caused by diarrhea. Switch to decaf versions of your favorite caffeinated drinks, like coffees, teas and sodas. Drink lots of water to compensate for the fluid loss caused by diarrhea — aim for 8 to 10 glasses per day. One of the dangers of diarrhea is it can cause dehydration.

Don't drink alcohol. Alcohol consumption can affect the ability of the body to absorb water. As the intestinal cells absorb alcohol, they lose their ability to absorb water because of the toxicity. This is because alcohol depresses the digestive tract’s movement. When the intestines do not absorb enough water to mix with the food, excess water will be left in the colon, leading to diarrhea. Remove alcohol from your diet completely to see if your IBS improves. If you you must drink, opt for a small glass of red wine instead of hard liquor or beer.
Consider a gluten-free diet. Your doctor may recommend you do a two week trail of a gluten-free diet. The insoluble fiber found in gluten — which is in rye, wheat, and barley — may worsen IBS symptoms. By cutting out gluten, you may find that your IBS improves significantly.

Stay away from fatty foods. Some people have difficulty absorbing fat, and unabsorbed fat can cause the small intestines and the colon to secrete more water, resulting in watery stool. Normally, the colon absorbs water from undigested, liquid foods in order to firm up the stool. But if the small intestines and colon secrete more water, the colon cannot absorb all of the water from the undigested liquid foods, resulting in diarrhea. Avoid fatty foods like fried foods, butter, cakes, junk food, cheese and other greasy foods.

Avoid foods that contain artificial sweeteners. Sugar substitutes such as sorbitol can lead to diarrhea due to their laxative effects. Sorbitol exerts its laxative effect by drawing water into the large intestine, thereby stimulating bowel movements. Artificial sweeteners are widely used in processed foods such as soft drinks, baked goods, powdered drink mixes, canned goods, candy, puddings, jams, jellies and dairy products. Always check the label before consuming.
Using Medications
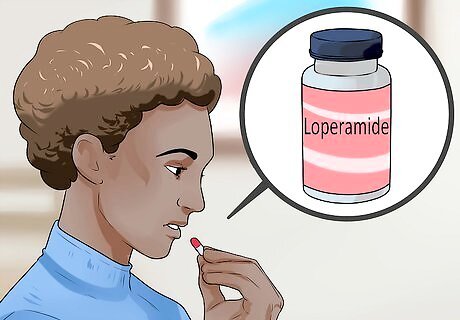
Take antimotility medicines. Loperamide is an antimotility medication usually recommended for IBS-related diarrhea. Loperamide works by slowing the contractions of muscles in your bowel, which slows down the speed at which food passes through your digestive system. This allows more time for your stools to harden and solidify. Some medications, including Loperamide, also increase the pressure of the anal canal, which helps with leakage. The recommended dosage of loperamide is 4 mg initially, with an additional 2 mg after each loose stool, but you should not exceed 16 mg over a 24-hour period.

Try antispasmodic medicines. Antispasmodics are a group of medicines that control gut spasms, reducing diarrhea as a result. The two main types of antispasmodic medicines appear to be equally effective in treatment of diarrhea caused by IBS. Antimuscarinics: Antimuscarinics or anticholinergics block the activity of acetylcholine (a neurotransmitter which is stimulates the stomach muscles to contract). This allows the muscles to relax, thereby relieving symptoms of abdominal muscle cramping. The commonly used antimuscarinic drugs are hyoscyamine and dicyclomine. For adults, the ideal dose is 10 mg taken three to four times per day. Smooth muscle relaxants: These work directly on the smooth muscle in the gut wall, allowing the muscle to relax. This relieves pain and prevents diarrhea. One of the most commonly used smooth muscle relaxants is alverine citrate. The usual dose for adults is 60-120 mg, taken between one and three times per day. If your diarrhea doesn't improve using one form of antispasmodic, try another.

Use painkillers to relieve cramping. Painkillers can be used to relieve the pain associated with abdominal muscle cramping. Painkillers work by blocking pain signals to brain. If the pain signal does not reach the brain, then pain cannot be interpreted and felt. Simple Painkillers: Simple painkillers are available over-the-counter and can be used to relieve mild to moderate pain. Examples include paracetamol and acetaminophen. Doses of simple painkillers may vary according to age, but the usual recommended dose for adults is 500 mg, every four to six hours. Stronger Painkillers: Stronger painkillers are usually only available by prescription and are used to relive moderate to severe pain. Examples include codeine and tramadol. Only take prescription painkillers according to your doctor's recommendations, as they can be addictive.

Get a prescription for antidepressants to relieve symptoms of IBS. In some cases, antidepressant medications can be used to treat IBS. Antidepressants block pain messages between the GI tract and the brain, thereby reducing visceral hypersensitivity (increased sensitivity of the GI tract nerves). Tricyclics (TCA's) and Selective Serotonin Reuptake Inhibitors (SSRI's) are the groups of antidepressants commonly prescribed for IBS. Consult with your healthcare provider for dosage recommendations as the ideal dosages of these medicines vary according to the manufacturer.
Managing Stress

Reduce your stress levels. Feeling worried, anxious, overwhelmed or tense stimulates colon spasms for people with IBS. The colon contains many nerves that are directly connected to the brain. These nerves control colon contractions. Stress results in abdominal discomfort, cramps, and diarrhea. Identify the source of stress. Knowing what's causing the stress in the first place will help you to avoid it. In IBS, the colon is more sensitive to even mild stress or anxiety. Taking on more responsibility than you can comfortably manage leads to increased stress. Know your limits and learn how to say when necessary. Find ways to express your feelings, which helps lower stress levels. Talking to open-minded friends, families and loved ones about any issues or problems you've been having can help to eliminate built-up stress. Learning effective time management skills helps avoid unnecessary stress.
Use hypnotherapy to decrease your stress. Hypnotherapy has may have a positive effect on patients with IBS. The form of hypnotherapist done in these sessions follows a 7–12 session gut-directed hypnotherapy protocol initially developed by PJ Whorwell. In these sessions, the patient first relaxes into the hypnotic trance. The patient then receives specific suggestions regarding GI functioning. The final phase of hypnosis includes imagery that increases the patient's sense of confidence and well-being. While this procedure has been shown to have positive outcomes, note that there is little evidence to show why it works. Hypnotherapy may work on patients unresponsive to other forms of treatment.
Schedule sessions with a therapist. Psychodynamic interpersonal therapy (PIT) offers detailed discussion of symptoms and the patient's emotional state. The therapist and patient together explore the links present between symptoms and emotional conflicts. One of the goals of PIT is to identify and resolve issues of interpersonal conflict that result in stress, and negatively impact IBS. PIT has been done most often in the UK. Field trials have shown a connection between PIT and relief from the symptoms of IBS. Usually, PIT is a longer-term treatment option. Studies show benefits coming only after at least 10 one-hour sessions, scheduled over the course of three months.

Try Cognitive Behavior Therapy (CBT) to address stress. Research shows that people with IBS who use CBT to learn behavioral strategies to manage their stress demonstrate significantly greater improvement than people who rely on medication alone. CBT works by teaching relaxation exercises, coupled with cognitive exercises to change existing belief systems and interpersonal stressors. CBT patients are taught to recognize existing patterns of maladaptive behaviors and responses to a variety of situations. For example, someone with IBS may believe their situation "will never change," thus leading to anxiety and stress. Using CBT, the patient learns to recognize the existence of this thought, and replace it with another, more positive belief. CBT is typically administered in 10–12 individual sessions. Group formats are also used.

Exercise more. Exercise lowers stress levels. In addition, new research suggests that exercise may help aid the digestive process. Exercise increases colonic motility (that is, the passage of wastes and other secretions through the colon), the length of time this passage requires, and the amount of transitive intestinal gas present in the colon. Aim for 30 minutes of moderate exercise five time a week or 30 minutes of vigorous exercise three times a week. Possible options include walking, bicycling, running, swimming, dance or hiking. If you aren't currently physically active, take it slow to start. Find an exercise partner or workout group. Share your workout goals on social media, where you may find support and encouragement. Exercise helps develop confidence, which in turn reduces stress.
Understanding IBS and Diarrhea
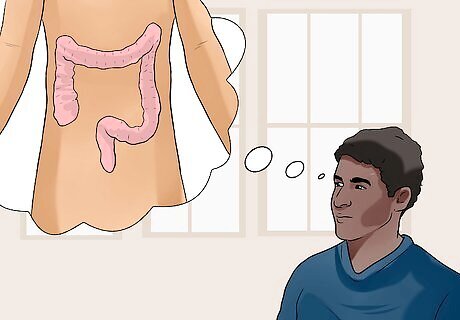
Educate yourself about IBS. Irritable bowel syndrome (IBS) is a disorder that affects the large intestine (colon). It commonly causes abdominal pain, bloating gas, cramping, constipation and diarrhea. For IBS patients, an increase in the sensitivity of the nerves in the GI tract (visceral hypersensitivity) can occur. This can develop after a gastrointestinal infection or after an operation that causes injury or damage to the nerves in the intestine. This results in a lower threshold for feeling intestinal sensations, therefore leading to abdominal discomfort or pain. Eating even small amounts of food may create discomfort as the stretch puts on the intestines. Fortunately, unlike more-serious intestinal diseases, irritable bowel syndrome does not cause inflammation or changes in bowel tissue. In many cases, a person with IBS can control the disorder by managing the diet, lifestyle and stress.

Familiarize yourself with the symptoms of IBS. While the most common symptom of IBS is diarrhea, there are a variety of symptoms that characterize this disorder. The symptoms vary widely from person to person. In addition, the symptoms may go away altogether for a time, before recurring with greater severity. Abdominal pain: Pain or discomfort in the abdominal region is one of the main clinical features of IBS. The intensity of the pain can be quite variable, from mild enough to be ignored, to being debilitating enough to interfere with daily activities. It is frequently episodic and can be experienced as cramping or as a persistent ache. Altered bowel habits: This is the most consistent clinical presentation in patients with IBS. The most common pattern is constipation alternating with diarrhea. Distention and Flatulence: Patients frequently complain of these unpleasant symptoms, which can attributed to increased gas. Upper GI symptoms: Heartburn, nausea, vomiting, and dyspepsia (indigestion) are symptoms that have been reported in 25-50% of patients with IBS. Diarrhea: Usually, diarrhea in IBS patients appears in between episodes of constipation (that may last from weeks to even a few months), but it can also be a predominant symptom. The stool may contain large amount of mucus, but never traces of blood (unless hemorrhoids are present). In addition, nocturnal diarrhea does not occur in patients suffering from this condition.

Rule out other possible causes of diarrhea. Diarrhea can be a symptom of many conditions besides IBS. Consider alternative diagnosis before IBS is claimed to be the cause of diarrhea. Proper diagnosis is required for appropriate treatment. Most commonly, an infectious agent is responsible for diarrhea. Salmonella or shigella are forms of food poisoning that result in diarrhea; however, these infections are usually accompanied by fever. Hyperthyroidism, malabsorption, lactose deficiency, celiac disease are other conditions which may cause chronic diarrhea.

















Comments
0 comment