
views
Changing Your Diet

Drink more fluids. Dehydration can worsen constipation by leading to hard, dry stools. When food waste passes through the colon, the colon absorbs water from the waste. If you are drinking adequate amounts of fluids, the colon will soak up less water from the food waste, resulting in softer stools. Try to drink about 8 full glasses of water a day, or about 2 litres (8.5 c). Start your day with 2 glasses right after you wake up, even before coffee. You should drink more water if you live in a very warm climate or when it's hot out. Be sure to also drink water while exercising to counteract the water lost through sweating. You may also need to drink more water as you increase your daily intake of fiber. If you suffer from heart or kidney problems and are receiving medical attention for either of these conditions, consult your doctor about your fluid intake before you make any major changes.
Increase your fiber intake. A healthy diet includes insoluble and soluble fiber. Soluble fiber helps the body to absorb more nutrients from the food you eat. Insoluble fiber does not break down in the body, but this type of fiber adds bulk and water to the stool, making it faster and more comfortable to pass the stool. Adults should aim to consume about 21-38 grams of fiber daily, depending on their age and sex. Women should eat 21-25 grams of fiber every day, while men require 30-38 grams. Sources of soluble fiber include oats, oat bran, apples, nuts, lentils and peas. Sources of insoluble fiber include wheat bran, seeds, almonds, whole grains, and most fruits and vegetables. Make sure to eat legumes and citrus fruits. In addition to fiber, these foods help colonic bacteria flourish which keeps the intestines healthier. Legumes in particular are among those foods that have the most fiber per serving. Incorporate prunes into your diet. Prunes are a good source of soluble and insoluble fiber and sorbitol, which has a natural laxative effect. Add more whole fruits and vegetables to your diet. Make sure you eat the skins on fruits and veggies, since the skin usually contains most of the insoluble fiber. Also be sure to eat whole fruits instead of fruit juices, which usually have less fiber and more sugar.

Cut back on low-fiber foods. These would include meat, ice cream, cheese, chips, meat, fast foods, and prepared and processed foods like hot dogs and frozen dinners. These low-fiber but high-fat foods may actually worsen constipation.

Avoid junk food. Fatty, sugary foods like cookies, crackers, cakes, and so on, tend to slow the digestive system down, since the gut is working to get all the calories it can from the fat in them. Try to avoid eating processed junk food.

Regulate your caffeine intake. Caffeinated drinks like coffee, tea, and soda have a diuretic effect and can lead to dehydration. However, caffeinated beverages can also promote contractions in the bowels and lead to bowel movements. In general, try to limit yourself to one cup of a caffeinated beverage per day, preferably in the morning to stimulate the bowels.
Making Other Lifestyle Changes
Get regular. Go to the bathroom at the same time each morning. Make this part of your morning routine because it is at this time that colonic motor activity is highest. In addition, the urge to have a bowel movement generally increases after you've had a meal, so try to take advantage of these natural signals from your body. Eat on a regular schedule to help "train" your body to regulate defecation. Try to eat your main meals around the same time each day. Your bowels love a routine! Since the mornings are peak times for bowel movements, make sure you eat high-fiber foods after you wake up. You may also want to include a hot drink (such as a cup of coffee) since warm beverages are calming and can help get the bowels moving.
Go to the bathroom when you need to go. Start listening to your body and don't ignore the urge to have a bowel movement because you want to wait until you get home or you want to finish the movie you were watching. The movements that trigger a bowel movement, called peristalsis, come and go, meaning that if you don't go immediately, that urge may disappear. The longer stool stays in the bowel, the harder it gets as more water is reabsorbed, usually resulting in a more painful and uncomfortable bowel movement when you finally have one.

Get in the right position. The position in which you try to eliminate stool can help you stimulate the bowels, although it is important to note that there is no right or wrong way to sit on the toilet. The following tips, however, might help make having a bowel movement easier and less painful: When you sit down on the toilet, place your feet on a small footstool. This helps to get your knees higher than your hips, which positions the rectum at such an angle that makes it easier to pass feces. Try leaning forward when sitting on the toilet. Rest your hands on your thighs. The leaning forward action will also help to get your rectum at a better angle. Try to stay relaxed and breathe deeply. Relax your anal sphincter to open your rectum and let the stool pass out.

Exercise. Many people experience an improvement in their constipation when they begin exercising or increase the amount of exercise they get. Doctors believe exercise helps food move more quickly through the large intestine. This means the colon has less time to absorb water from the stool. Aerobic exercise increases breathing and heart rate which can also stimulate the intestinal muscles to contract, which is an important factor in moving stools through the intestines. Do an aerobic exercise that gets your heart rate up for a period of at least 20-30 minutes, 3-4 times a week. If you can, try to do some exercise every day, even just walking for 15-20 minutes. Daily exercise will hopefully stimulate daily bowel movements because as you become active so do your bowels. Incorporate a more intensely aerobic exercise or non-competitive sports into your routine if you are already moderately active. Try running, swimming, or aerobic classes. Abdominal strengthening exercises can also help stimulate the muscles in the digestive system.
Catch up on your sleep. Lack of adequate sleep over a long time aggravates constipation and can lead to a more severe condition. Try to get between 7-8 hours a night of restful sleep. The bowels can also "sleep " night, so when you wake up, you may be able to have a bowel movement since that is the peak time!

Relax your mind. Because mental stress can interfere with relaxation of the whole body, including the bowels, it's important to use some type of relaxation technique daily. Doctors believe that some patients cannot push properly when having a bowel movement because they feel rushed and stressed out. In other words, stress increases constipation. Take up relaxing activities like yoga, meditation, swimming, etc. Read a book or watch a movie to escape to another world.
Taking Laxatives
Use bulk-forming agents (or fiber). Fiber helps absorb fluid in your intestines and make your stool bulkier, which in turn helps the bowels contract and push the stool out. It is important, however, that you try to incorporate more fiber into your diet before trying a supplement as this is truly the best way to get more fiber. Most bulk-forming agents can be taken in capsule or powder form and mixed with 8 oz of water or fruit juice. Follow any directions on the label and only take the recommended dosage. Potential side effects include increased flatulence, cramping, and bloating. Most people see results within 12 hours to 3 days Common bulk-forming laxatives include: Psyllium - Psyllium is a soluble fiber used to increase bulk and stimulate the bowels to contract and release stool with ease. A significant amount of research has suggested that psyllium can relieve constipation. You can find psyllium in the widely available product Metamucil. You must drink at least 8 oz of liquid when you take psyllium. Polycarbophil - Polycarbophil calcium has been shown in several studies to help treat chronic constipation.

Take lubricant laxatives. With the main ingredient being mineral oil, lubricants work by coating the surface of stool, which helps the stool keep fluid and pass more easily. Most people see results within hours of consumption. Popular brand names available in most pharmacies include Fleet and Zymenol. Lubricants are simple and inexpensive laxatives, but should only be used as a short-term prescription. The mineral oil in lubricants can decrease the effectiveness of certain prescription drugs and can also inhibit the absorption of fat-soluble vitamin and minerals in your body. Lubricant laxatives are generally taken at bedtime and may be taken orally on an empty stomach and in an upright position. Be sure to drink at least 8 oz of water or juice after you take this laxative. Physicians do not recommend mineral oil for persistent treatment of constipation.

Take emollient laxatives. Better known as stool softeners, emollient laxatives, such as Colace and Docusate, work to increase the amount of water in the stool and to thereby soften it. These laxatives take longer to work (usually 1-3 days) but are commonly used by those who are recovery from surgery, women who have just given birth, and individuals suffering from hemorrhoids. Stool softeners come in capsule, tablet, and liquid form, and are generally taken at bedtime. Follow any directions on the label and take only the recommended dosage. Make sure to take capsules and tablets with a full glass of water. For liquid stool softeners, there should be a marked dropper that helps you measure the exact dose. Ask the pharmacist for help if you're not sure how to use it. Mix the liquid 4 oz of juice or milk to mask its bitter taste and to make it easier to get down.

Take osmotic laxatives. Osmotic agents help your stool retain fluid and increase the number of bowel movements. Osmotic laxatives include Fleet Phospho-Soda, Milk of Magnesia, and Miralax, all of which work to draw fluid into the intestines from surrounding tissue. Potential side effects include dehydration, gas, cramps, and a mineral imbalance in your system. Older adults and people with existing heart or kidney problems should be careful when taking osmotic agents because of their dehydrating properties. Osmotic agents come in pill or powder form. Miralax, for example, is a powder that should be dissolved in 4-8 oz of water or fruit juice. The bottle comes with a measure device so that you can take the appropriate dosage (17 g). You can also buy single-dose packets. Follow any other directions on the bottle and only take the recommended dosage.

Take stimulant laxatives. Stimulant laxatives cause the intestines to contract, which moves stool quickly and pushes it out. You should only use stimulants if your constipation is severe and you feel like you require immediate relief. Stimulant laxatives should not be used on a continuing basis to treat chronic constipation. You should see results within 6-10 hours. Popular brands include Ex-Lax, Dulcolax, and Correctol. These laxatives can cause cramping and diarrhea. Stimulant laxatives can be taken orally (in pill, powder, or liquid form) or as a rectal suppository. Always take stimulant laxatives as directed and take only the recommended dosage. This type of laxative is generally taken at bedtime. Stimulant laxatives are the harshest laxatives on the body. They should not be used regularly or daily because they can weaken the body's ability to have a bowel movement on its own. They can also limit your body's ability to absorb vitamin D and calcium. Consult your physician if you're using these laxatives for more than one week.

Try natural or herbal laxatives. There are also a number of remedies to relieve constipation that involve household ingredients and/or herbs. However, you should note that many of these are not supported by strong scientific research. Consult with your pediatrician before giving any of these remedies to your child. Some of the most popular natural or herbal remedies for constipation include: Aloe vera - Aloe juice or aloe latex, a yellow, bitter liquid derived from the skin of the aloe leaf, is a powerful laxative and can stimulate bowel movements. However, it can cause painful cramping and physicians do not recommend its use as a laxative. Blackstrap molasses - Mix 2 teaspoons (9.9 mL) of blackstrap molasses in 1 cup (240 mL) of warm water. Then drink up. Blackstrap molasses is rich in magnesium, which helps ease bowel movements. Lemon juice - Lemon juice helps to cleanse the intestine and induce bowel movements. Add 1 teaspoon (4.9 mL) of lemon juice to 1 cup (240 mL) of warm water and add a pinch of salt. Drink the solution on an empty stomach.

Note that all of these OTC treatments should only be temporary. If you find yourself using a laxative for more than 1 week, you should consult your physician. Laxative abuse can actually worsen constipation, as your body may come to rely on the laxative in order to pass a stool. Never use laxatives to be "regular". Always try to incorporate more fiber into your diet first.
Understanding Constipation
Understand that chronic constipation is common and has multiple causes. Chronic constipation affects between 15% and 20% of Americans. Even people who eat healthily, exercise, and drink lots of water can still suffer from chronic constipation. Lifestyle issues - Constipation has been related to a number of factors related to lifestyle and diet, including inadequate water intake, inadequate fiber intake, over-consumption of dairy, and a lack of exercise, among others. Existing or new medical conditions - Some medical conditions can cause changes in the bowels and chronic constipation, including colon cancer, hypothyroidism, irritable bowel syndrome, Parkinson's disease, and diabetes. Medications - Medications that often have constipation as a side effect include pain medications, antacids like calcium and aluminum, calcium channel blockers, iron supplements, and diuretics among others. Aging - As people get older, they become more sedentary (and get less physical activity), eat less fiber and drink less water, all of which contributes to chronic constipation. In addition, many over-the-counter and prescription medications taken to treat conditions more common in older people, such as arthritis, back pain, and hypertension, can cause chronic constipation. Psychological issues - For some people, chronic constipation is related to specific psychological issues, including depression, sexual or physical abuse, or loss of a family member or friend, among other emotional triggers. Nerve and muscle function in the bowels - In some cases, lack of proper nerve and muscle function can cause constipation. In particular, in cases of pelvic floor dysfunction (dyssynergic defecation), the muscles of the lower pelvis surrounding the rectum do not function properly and can cause constipation.

Take note of your symptoms. Some physicians believe that chronic constipation cannot solely be determined by the frequency of bowel movements, but that a host of other symptoms need to be assessed, or what has been termed a "symptom complex". These include: Hard stools. Excessive straining when having a bowel movement. A lack of feeling of relief after a bowel movement or a sense that the bowel movement was incomplete. A sensation that you are unable to have a bowel movement. A decrease in frequency of bowel movements (fewer than 3 per week over a period of several months)
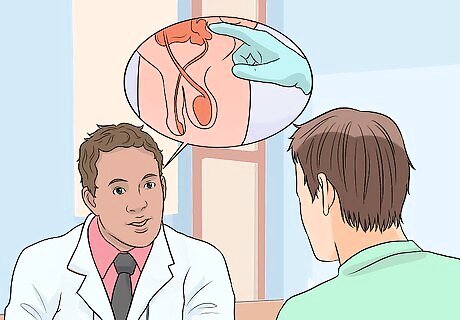
Make an appointment with a doctor. If the dietary and lifestyle changes discussed above do not relieve constipation, consult your primary care physician. It's important to seek medical attention if you suffer from chronic constipation or if constipation is new to you, as it can be a symptom of a more serious medical condition. Be prepared to provide your doctor with information on your constipation, including the number of times per week you pass a stool, how long you have experienced difficulty defecating, and a list of any medications you may be taking. Be sure as well to tell your doctor of any treatments you have undertaken, including laxatives and lifestyle or dietary changes. Your doctor will perform a rectal examination to check for tears, hemorrhoids, and any other abnormalities, and then do laboratory testing to screen you for different diseases and conditions. If after these tests and a comprehensive medical history interview the cause of your constipation is still uncertain, your doctor may order an imaging study of the colon and rectum to check for more serious problems, such as an obstruction. In severe cases, your doctor may order more tests or refer you to a gastroenterologist for further evaluation.



















Comments
0 comment