
views
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
It might sound scary, but many people with this condition never experience any symptoms, while others have mild discomfort, belching, and heartburn. Experts note that if you start paying attention to the common symptoms, you can visit your doctor for a diagnosis through a medical test.[2]
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
After that, you can work with your doctor to create a treatment plan.
Recognizing Symptoms and Causes of Hiatal Hernias

Pay attention to heartburn. The stomach is a very acidic environment because it must mix and break down food while fighting off harmful bacteria and viruses. Unfortunately, the esophagus cannot handle acidic material. A hiatal hernia can cause backflow of food into the esophagus, which results in a burning sensation. Since this occurs near the heart, it's called heartburn.
Be alert if you have difficulty swallowing. During heartburn, the esophagus becomes filled with food from the stomach. This can prevent you from swallowing normally. If you find that you're having trouble swallowing food or drink, see your doctor.
Take note if you regurgitate food. Sometimes, the acidic contents of your stomach reach the top of your esophagus and leave a bitter taste in your mouth. A hiatal hernia can also cause actual regurgitation, which is essentially throwing up in your mouth. This could be a sign of a hiatal hernia.
Seek immediate help if you have chest pain or other severe symptoms. Sometimes a large hiatal hernia might cause your chest to hurt. You might also vomit blood, which can indicate gastrointestinal bleeding. If you suffer from these symptoms, seek medical attention immediately.
Know the causes of hiatal hernias. When you're trying to determine if you have a hiatal hernia, it can be useful to know some common causes. They may be the result of trauma to that area, changes to your diaphragm as you grow older, or persistent pressure, such as vomiting or coughing. Many hiatal hernias do not have a clear cause. The weakened muscle tissue that allows a hiatal hernia to develop can happen for unknown reasons. If you do identify with one of the common causes and also suffer from symptoms, talk to your doctor about whether you might have a hiatal hernia.
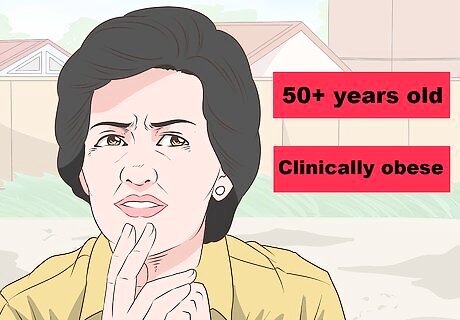
Understand the risk factors. Some people are at greater risk for developing a hiatal hernia. If you are concerned that you might have one, consider whether either of the following applies to you: You are over 50 years of age. You are clinically obese.
Getting a Medical Diagnosis
Talk to your doctor about your symptoms. Schedule an appointment with your doctor if you suspect you have a hiatal hernia. Only medical tests can definitively diagnose a hiatal hernia. Talk to your doctor about any of the symptoms you've been having. Keep track of your symptoms before your appointment so that you can be as specific as possible. While investigating for a hiatal hernia, your doctor may have you start taking medication for heartburn control.
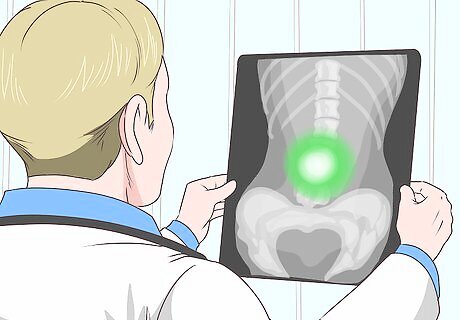
Get an X-ray. Your doctor might use 1 or several tests to determine whether or not you have a hiatal hernia. One of the simplest tests is an X-ray. Your doctor will have you drink a chalky liquid so that they will be able to view your esophagus, stomach, and upper intestine clearly in the X-ray.
Schedule an upper endoscopy. Your doctor may choose to rely on an upper endoscopy in addition to, or instead of, an X-ray. During this procedure, your doctor will insert a thin, flexible tube into your throat. There is a camera on the end that captures pictures of your esophagus, which your doctor will use to make a diagnosis. You will likely have to schedule a separate appointment with a specialist, as your GP is unlikely to do this in their office. Ask to be sedated if you are nervous about this procedure. It's not painful, but it can be unnerving to many people.
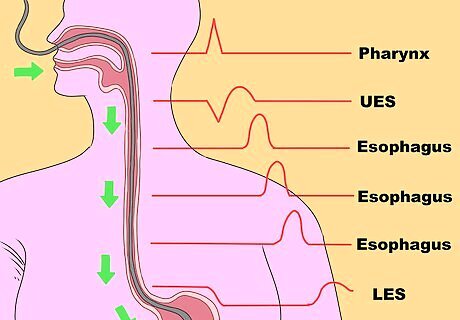
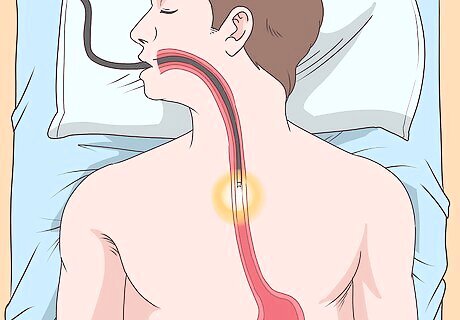
Have your doctor perform an esophageal manometry test. Your doctor might order this test in addition to others. A manometry measures how effectively you can swallow food and liquids. This helps determine the severity of the hiatal hernia. During this test, the technician will place a thin tube through your nose, down your throat, and into your stomach. You'll drink small amounts of water with the tube in place to measure your ability to swallow. This test is not painful, but it might be uncomfortable or unpleasant.
Discussing Treatment Plans with your Doctor
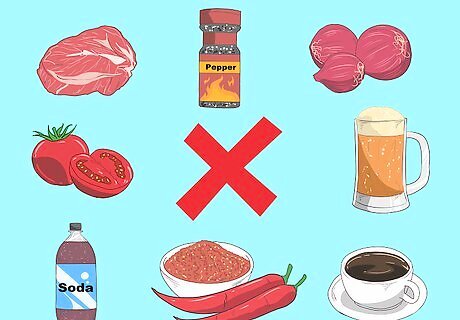
Try dietary changes as a first step. Once your doctor confirms that you have a hiatal hernia, work together to develop a treatment plan. This treatment plan will start with lifestyle changes to see if it is possible to manage your symptoms without surgery. For example, you can try managing your symptoms by altering your diet. Avoid eating: Fried and fatty foods. Foods that contain caffeine, including coffee and chocolate. Highly acidic foods, such tomatoes. Spicy foods. Peppermint or spearmint. Onions. Red meat. Carbonated beverages and alcohol.
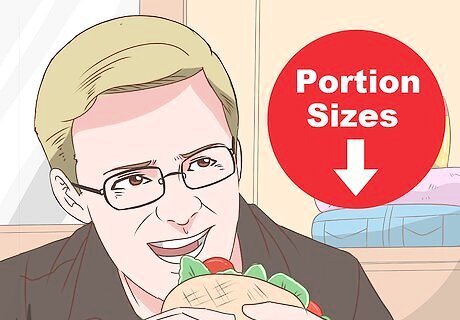
Change your eating habits for added relief. Making some changes to your routine can help manage symptoms. Start by decreasing the portion sizes of your meals, and make sure to eat at least 3-4 hours before lying down. This will help to reduce symptoms like heartburn or regurgitation.
Take over the counter medications to reduce symptoms. Your doctor might recommend medications to offer extra relief from your symptoms. Consider taking antacids or H2-blockers, such as Zantac. Make sure to follow the dosage instructions. Call your doctor if symptoms don't improve after 2 weeks. They might prescribe something stronger, such as Nexium or Prilosec. Carefully follow instructions for prescription medications, too.
Consider surgery if lifestyle changes don't help. In extreme cases, surgery is necessary to repair a hiatal hernia. If your symptoms are still causing you problems after lifestyle and dietary changes, talk to your doctor about surgical options. During the operation, the surgeon will pull the stomach back into the abdomen and also close the hole in the diaphragm muscle. Talk to your doctor about whether this is the right choice for you, and also ask about the recovery process.













Comments
0 comment