
views
Identifying Asthma Symptoms

Understand the different symptoms. Make sure your teen understands the different signs and symptoms of an oncoming flare-up or attack. Asthma symptoms include coughing, wheezing, chest tightness, and shortness of breath. Coughing caused by asthma is often worse at night or early in the morning. This can make it difficult to sleep. Wheezing is a squeaking or whistling sound that occurs when you breathe. Chest tightness feels as if something is squeezing or sitting on your chest. Shortness of breath feels as if you cannot catch your breath, or cannot get air out of your lungs. You will generally feel out of breath.
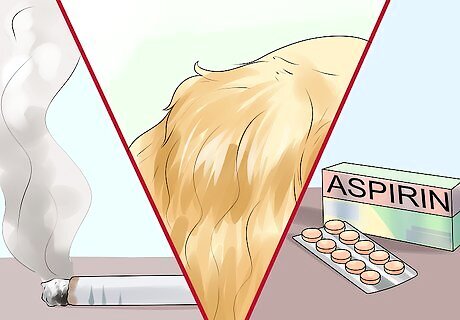
Know what can trigger an attack. Many different things can trigger or worsen asthma symptoms. Triggers include allergens, irritants, medicines, sulfites in foods and drinks, viral upper respiratory infections, and physical activity. Other health conditions, such as a runny nose, sinus infections, reflux disease, psychological distress, and sleep apnea, can trigger an attack and make asthma harder to manage. Allergens include dust, animal fur, cockroaches, mold, and pollens from grasses, trees, and flowers. Irritants include cigarette smoke, air pollution, sprays (like hair spray), chemicals or dust, and compounds in home décor products. Medicines include non-steroidal anti-inflammatory drugs (NSAIDs), like aspirin, and nonselective beta-blockers.
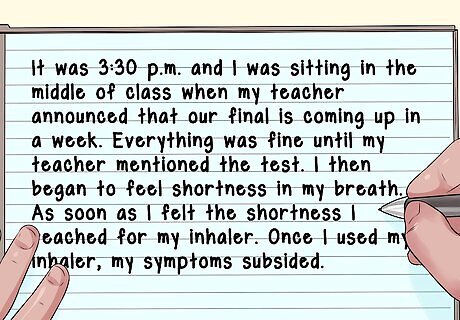
Keep a diary. Encourage your teen to keep a diary detailing when the flare-up occurred (for example time of day), what they were doing, their surrounding environment, and the medicines they took to control the flare-up. This way, your teen can identify specific triggers in order to avoid them. A diary will also help your teen determine how well their medicine is controlling their asthma. For example, “It was 3:30 p.m. and I was sitting in the middle of class when my teacher announced that our final is coming up in a week. Everything was fine until my teacher mentioned the test. I then began to feel shortness in my breath. As soon as I felt the shortness I reached for my inhaler. Once I used my inhaler, my symptoms subsided.”

Contact their doctor. The doctor will diagnose the asthma based on your teen's medical and family history, test results, and a physical exam. Your teen's doctor will also diagnose the severity of asthma, i.e., intermittent, mild, moderate, or severe. Then, the doctor will formulate a treatment plan based on the severity of the asthma. Let the doctor know whether your teen's symptoms happen during a certain time of the day, at certain places, or if they get worse at night. Have your teen bring their asthma diary for the doctor to review. Doctors use a test called the spirometry to check how well the lungs are working. The doctor may also recommend allergy tests, chest x-rays, and tests to rule out other diseases that have similar symptoms to asthma like sleep apnea, vocal cord dysfunction, or reflux disease.
Create an asthma action plan. With their doctor, create an asthma action plan with your teen. The asthma action plan should detail asthma triggers and the different levels of severity of an asthma attack. It should outline symptoms and peak flow measurements that indicate a flare-up or worsening asthma, as well as specific medicines to take based on their signs, symptoms, or peak flow measurements. The action plan should also outline symptoms or peak flow measurements that indicate the need for urgent medical attention. The plan should also include telephone numbers for emergency contacts, your healthcare provider, and your local hospital. Encourage your teen to carry their action plan with them wherever they go. You can find an action plan template here: http://teenshealth.org/en/teens/action-plan-sheet.html?WT.ac=ctg.
Teaching Your Teen to Use a Peak Flow Meter

Move the indicator to the bottom of the scale. Tell your teen to stand up and to take a deep breath. Make sure your teen fills their lungs with air all the way, like a balloon.
Have your teen place the mouthpiece in their mouth. While your teen does this, make sure they hold their breath. Also, make sure they place the mouthpiece between their teeth. Then, have them seal their lips around the mouth piece. Make sure they do not place their tongue inside or against the hole.

Blow out. In a single blow, tell your teen to blow out as fast and as hard as they can. Remember that the most important burst of air is the first burst of air. You cannot correct this by blowing for a longer time. However, if they coughed or did not blow hard or fast enough, have them redo steps one through three again.
Have them write down their score. In order for them to find their peak flow number, they will need to repeat steps one through three twice more. Have them record the number each time. The number that ranks the highest will be their peak expiratory flow (PEF). Make sure they record their peak flow number in their asthma action plan.
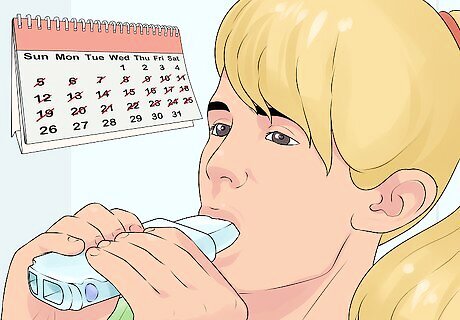
Find their personal best. In order for them to find their personal best, have your teen take their peak flow each day for two to three weeks. The highest number they get over the two to three week period is their "personal best" PEF. Make sure they do not take their measurement if their asthma isn’t under control. Advise them to use the peak flow meter two times per day around the same times each day, and as instructed by the healthcare provider.

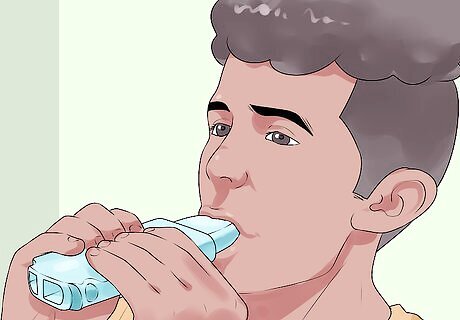
Use it every day. Once your teen knows their personal best, help your teen develop a habit of using the meter to track their breathing. Your teen should use the meter every morning before they take their medicine, when they are experiencing asthma symptoms or an attack, and after they have taken their medicine for an attack or the presence of symptoms. Have your teen check to see which zone their number is in, and what actions to take depending on their action plan.
Dealing with Flare-Ups

Pay attention to the signs. When your teen notices any signs or symptoms of an oncoming attack, they should tell someone that a flare-up is about to happen, or let people around them know what is going on. Advise them to sit down and take slow, steady breaths. Symptoms of an oncoming attack are a cough, breathlessness, wheezing, tightening of the chest, difficulty speaking or eating, and increased or rapid breathing. For example, if they are at school, tell them to let their friends, teachers, coaches and/or school nurse know what is going on. Make sure the school nurse has your child's action plan on record and an extra rescue inhaler.

Follow the action plan. Have them revert immediately to their action plan. Remind them to remain calm and follow the action plan’s protocol. To help your teen act swiftly in a situation, do practice runs at home. Practice for each asthma zone, i.e., the green, yellow, and red zones. Practicing at home will help your teen feel confident that they can control and prevent a full attack even if they do not have their action plan with them.

Remove the trigger. If they can figure out what triggered the attack, then encourage them to remove the trigger, or remove themselves from the area. Remind them to not ignore a flare-up in hopes that it will go away on its own. It needs to be dealt with promptly in order to prevent an emergency situation. Advise them to call an ambulance (911) if they don't have their inhaler or medication with them, if their symptoms do not improve after 10 puffs, if they feel worse despite using their inhaler, or if they are worried at any point. If the ambulance takes longer than 15 minutes, then have them repeat step two.



















Comments
0 comment