views
Helping Process the Emotions of Parkinson's

Educate yourself about the disease. Parkinson's effects and treatment can be complex. Learn as much as you can from the patient's doctor, Parkinson's support groups, or books, and share what you learn with your loved one as well. The National Parkinson's Foundation, American Parkinson's Disease Association, and The Michael J. Fox Foundation are excellent resources for Parkinson's patients and their families.

Communicate openly. Some people with Parkinson's keep their diagnosis a secret for a while, while others are more open. Do your part by communicating openly. Don't treat the diagnosis like a secret or an embarrassment. Instead, embrace it as the key to getting the information you and your loved one need to cope. Encourage your loved one to express their emotions. Encouraging positivity doesn't mean burying the more painful feelings. If they say "I'm frightened," you can say "I hear you" instead of "Everything will be fine!" The better the relationship between the person with Parkinson's and their primary caregiver, the better the outlook in terms of depression and physical health. If you are loving, caring, and concerned, you are helping. This doesn't mean you should neglect yourself! Be open about how you are feeling, and make sure you get the care you need.

Notice changes in emotion. Depression is a clinical symptom of Parkinson's, and the sufferer should report it to their doctor. If you notice that someone with Parkinson's has grown withdrawn, moody, or sad, let them know. Tell anyone else involved in their care what you have observed. Parkinson's causes a deficiency in dopamine, so any mood shifts are a possible sign of a change in that department. The doctor will likely want to treat the depression with medication if it is diagnosed. Offer to go with the doctor with them if they will let you.

Visit a support group. There are support groups for those with Parkinson's and for their caregivers, to attend either separately or together. These can be of great benefit for you both. Parkinson's can lead to feelings of isolation, and caring for someone with Parkinson's can be mentally depleting and socially isolating as well. Try going together or separately. Ask your doctor about local groups. Online forums can also be helpful—search for one that you like.
Being a Primary Caretaker
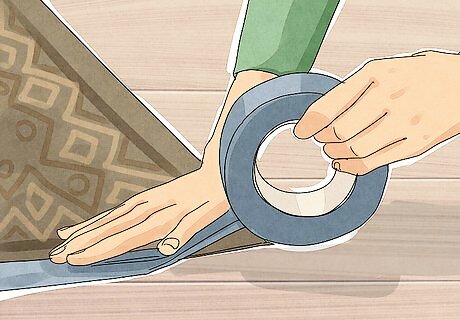
Make safety changes to the home. Since the disease becomes progressively more severe, take precautions in advance to lower the risk of falls: Free up floors from clutter and remove loose rugs. If your loved one finds it difficult to walk smoothly on thick floor rugs, replace them with thin carpet or solid flooring. Install safety rails, raised toilet seats, and tub chairs. Grab bars are especially important next to the toilet and in the shower. Install a non-skid mat in the shower. Stabilize furniture so it won't tip over when grabbed for support. Remove tall lamps, floor vases, side tables, and other unstable furniture.

Attend doctor's visits. As long as your loved one allows, attend doctor's visits with them. It is hard for someone with Parkinson's to notice all the changes they are going through, or to remember everything they are instructed to do at the appointment. Go along, and take notes.

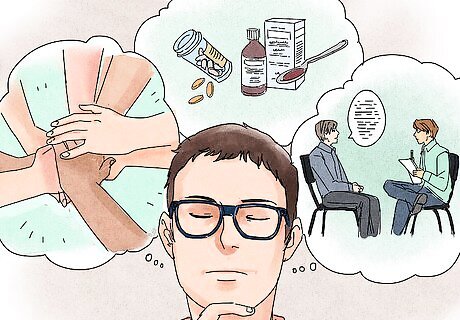
Ask about drug treatments. Parkinson medication can be complex, and what works for one person may not work for another. Options include levodopa, dopamine agonists, COMT inhibitors, and MAO-B inhibitors. Talk to your loved one and to the doctor regularly about how the treatment is going. Don't hesitate to ask the doctor about alternatives or to bring up concerns you have with the current treatment. If these treatments are not effective enough or if the disease progresses to the late stages, there are several surgical treatments available as well.
Keep a schedule, but expect it to change. When someone is going through Parkinson's, there's a lot to fit in: medications, doctor's visits, exercise routines…and the ordinary social events and chores that make up normal life. Keep extra time in your schedule whenever you are planning activities that involve your loved one, as they will experience fluctuations in mood and energy which can make it hard to schedule some activities in advance.

Support the independence of your loved one. It's important to let Parkinson's sufferers do what they are capable of doing. Taking over all tasks for fear they might slip up can make it worse for them. Keep an eye on how they are doing, but do let them self-direct as normal until it becomes too dangerous. Before you offer help, ask. Especially in the early stages, ask for permission before touching or otherwise guiding someone with Parkinson's.

Start movement therapy early. Exercise, physical therapy, and activity is helpful for those with Parkinson's, and the earlier it starts, the better. Cardiopulmonary fitness is crucial: exercises like treadmills walking at varying inclines, hiking with walking sticks, and swimming (with a variety of strokes) are excellent choices. Exercise that includes changes of tempo or action is beneficial for the cognitive maintenance of those with Parkinson's. Suggest that your loved one try walking in public places, doing yoga or Tai Chi, and taking classes where an instructor leads them through a series of exercises.

Talk to the patient's doctor and dietitian about nutritional needs. There is not yet evidence of a specific "Parkinson's diet" that will help all patients, but a healthier diet may improve overall well-being and make it easier to cope. With medical advice, you can also explore possible dietary changes to treat certain problems. For example: If medication causes constipation, increase fiber and fluid intake. Levodopa or L-dopa, a common Parkinson's drug, may not be absorbed properly if taken with protein. If the patient is prescribed L-dopa, talk to their doctor about eating protein at certain times of day, or in smaller amounts. Do not change the diet without checking with the doctor. There have been many studies suggesting a link between diet and Parkinson's, but few clear results. Talk to the patient's doctor about the latest medical research.

Get compression stockings to prevent dizziness. Mid- to late-stage Parkinson's can cause a sudden drop in blood pressure when the patient stands up. This condition, called orthostatic hypotension, can cause dizziness or even fainting, potentially leading to a bad fall. Wearing compression stockings or abdominal binders while sitting or lying down can help by preventing blood from pooling into the patient's legs. The patient's doctor can suggest additional treatments if this is still a problem.

Seek ongoing support. The person with Parkinson's will experience new challenges and find new ways to cope with them. In addition to continuing exercise, social interaction, and medical treatments, it may help to seek counseling support, or alternative therapies such as acupuncture or meditation. Do not take herbal remedies without consulting a doctor first. Some herbal remedies may interfere with medication.
Helping Out in Little Ways

Check in regularly. Someone with Parkinson's may be experiencing changes frequently, and may not even notice all of them. If you check in regularly, you'll get a good sense of how they are changing. Try calling or stopping by once a week if you are a friend, or come by every day if you are closer and your schedule permits (as long as this many visits are welcome!). If you do notice concerning changes, or see new difficulties that could be solved with adjustments to the household, do mention what you see to the person with Parkinson's or to a caretaker. Look for new needs. If your friend can no longer drive, offer to drive them to appointments or to the grocery store.

Offer to join in on walks and social activities. People with Parkinson's benefit from walking and walking-based exercises. Depending on how they are doing, they may be able to hike, walk in a mall, or walk very slowly. In the latter scenario, you may have to help them at some points or just be patient as they put one foot in front of another. Social interaction is also beneficial.

Do what you used to do. Insofar as a friend or loved one with Parkinson's is still capable, keep inviting them to do what you did before. They may need extra support to do it, so make changes to accommodate this!
Make long-term plans. The course of the disease varies from person to person, but generally starts with mild symptoms. It can eventually progress to the most advanced stage, that may leave the person bed- and wheelchair-bound. Make plans in advance so the transition, if it comes, is less stressful.



















Comments
0 comment