
views
X
Trustworthy Source
National Institute of Diabetes and Digestive and Kidney Diseases
Health information from the National Institute of Diabetes and Digestive and Kidney Diseases, a division of the U.S. National Institutes of Health
Go to source
In most cases, the condition can be relieved by practicing certain techniques at home, but sometimes emergency medical intervention is needed.
Improving Bladder Emptying at Home

Strengthen your pelvic muscles. One of the most effective and best-known ways of strengthening your pelvic floor muscles is by doing Kegel exercises. They are simple exercises you can do anywhere that increase the strength of the muscles that control your bladder — as well as the uterus, small intestine and rectum. To help identify your pelvic floor muscles, stop urinating in midstream. The muscles that contract are the ones Kegel exercises strengthen. The exercises can be done in any position (so you can do them while sitting at traffic, at your desk at work, etc.), although it's easier while laying down. Once you've identified your pelvic floor muscles, tighten them and hold the contraction for five seconds, followed by relaxing them for five seconds. Repeat this sequence five to 10 times a few different times daily. Over the course of a few weeks, work up to keeping the pelvic muscles contracted for 10 seconds at a time, while also relaxing for 10 seconds afterwards. Do the exercises standing and sitting as well. Repeat this sequence five to 10 times daily until you're able to control your bladder better. Be careful not to cheat by flexing your abdominals, thighs or buttocks, and remember to breathe freely while doing the exercises. Many factors weaken pelvic floor muscles, such as pregnancy, childbirth, surgery, aging, obesity, chronic coughing and excessive straining from constipation.

Retrain your bladder. Bladder training is an important behavioral therapy that can be effective in treating urinary retention and incontinence. The goals of this therapy are to increase the amount of time between urinating, increase the volume of fluid your bladder can hold and diminish the sense of urgency and/or any leakage issues. Bladder training requires that a fixed bladder emptying schedule be established, regardless if the urge to urinate is present or not. If the urge to pee occurs before the assigned time, urge suppression via contracting the pelvic muscles should be done. Empty your bladder as best you can as soon as you wake up. Then set intervals of one to two hours to try to go again, regardless of urge. As success is achieved controlling your bladder and urinating on demand, increase the interval in 15–30 minute increments until it's possible to remain comfortable for three to four hours. It typically takes between six to 12 weeks to gain control of your bladder again and be able to fully void it when you feel the urge to urinate.

Make yourself comfortable in the bathroom. Making yourself comfortable in the bathroom can contribute to being able to empty your bladder normally. If the air temperature or floor is too cold, that could distract you from the business at hand. Sitting down on the toilet may be the most comfortable for both genders, as some men feel back, neck or prostate pain while standing to urinate. Privacy can also be an important comfort factor, so don't try to urinate in public bathrooms and keep the door shut while at home. Turn the temperature up in your house during the winter time and consider wearing slippers and a robe to the bathroom to keep warm. Set up some aromatherapy candles in your bathroom and give it a "spa look" to soothe and relax you while you're trying to pee. If you're a "clean freak," keep your bathroom tidy so it doesn't distract or bother you. Take your time. You need to allow yourself an average of 30–60 seconds to urinate, so don't rush and get stressed about it. Try running some water in the bathroom sink in efforts to stimulate a strong urge to empty your bladder.
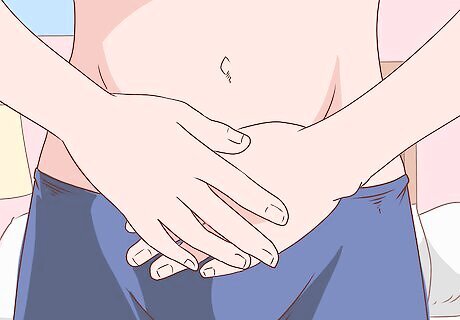
Apply external pressure or stimulation. Applying pressure over your bladder from the outside of your lower abdomen can help stimulate urination and promote full emptying of the bladder — think of it as a kind of massage or physical therapy. Look online to get an anatomical understanding of where your bladder is, then apply gentle pressure inward (towards your spine) and downward (towards your feet) to try and "milk" your bladder while urinating. This technique is easier to do while standing, as opposed to sitting on the toilet hunched forward. Alternatively, try tapping the skin/muscle/fat directly over your bladder to trigger a contraction and release. For women, inserting a sanitized finger into their vagina and applying forward pressure against the anterior vaginal wall can often stimulate the bladder and get it to release urine. For men, too much stimulation of the lower abdomen might cause an erection, which makes it much more difficult to urinate. As such, maintain a flaccid penis when trying to fully empty your bladder. Letting warm water run over your lower abdomen and genitalia can trigger the urge to pee. As such, try emptying your bladder while taking a warm shower.
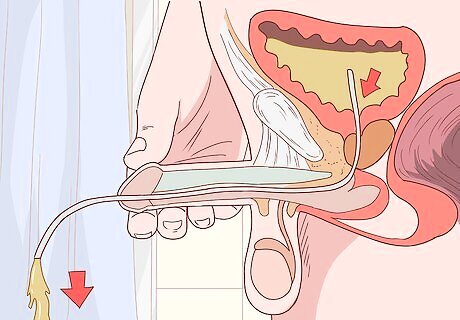
Learn about self-catheterization. If you're really desperate to urinate and are feeling significant bladder and kidney pain, then self-catheterization may be the answer if the above advice doesn't work. Self-catheterization involves inserting a catheter (long, thin tube) up into your urinary tract and close to the opening of the bladder in order to drain urine from it. This procedure needs to be taught and demonstrated by your family doctor or urologist, but it's not for the squeamish or faint of heart. It's usually better for your doctor to perform catheterization under a local anesthesia, but if you feel comfortable with the procedure and can use some lubrication instead, then give it a try. Lubrication can reduce the need for a topical anesthesia, but some compounds (such as petroleum jelly) can irritate the delicate mucus membranes of the urethra and lead to pain. It's important to sterilize the catheter thoroughly before inserting it into your urethra, as any introduction of bacteria can lead to an infection.
Getting Medical Treatment

Consult with your doctor. If you're having trouble emptying your bladder for more than a few days consecutively, then make an appointment with your family doctor. Your doctor will examine you and try to find the root cause. In addition to weak pelvic muscles, other causes of urinary retention include: blockage in the urethra, bladder/kidney stones, genitourinary infections, severe constipation, cystocele formation (in women), prostate growth (in men), spinal cord injury, over-use of antihistamines and after effects from anesthesia due to surgery. You doctor may take a urine sample, x-rays, CT scan, MRI and/or diagnostic ultrasound studies to determine the cause of your bladder problem. Get a referral to a genitourinary specialist for more testing, such as cystoscopy (insertion of a scope to view inside the bladder/urethra), urodynamic testing (measures bladder's ability to empty), and/or electromyography (measures muscle activity of bladder/lower pelvis). Common symptoms of urinary retention include: pain in lower abdomen, bloating, frequent urge to urinate, difficulty starting/stopping urine stream, weak flow of urine and leakage. If you're in severe discomfort from a full bladder that refuses to empty, your doctor can drain your bladder with a catheter — a relatively quick outpatient procedure done with a local anesthetic. Self-catheterization can be taught for home use (see above).
Ask about available medications. Ask your doctor if your bladder problem and inability to void urine normally can be treated with medication. Some drugs can cause dilation (relaxation and widening) of the smooth muscle of the urethra and opening of the bladder, although long-term use of these can cause the opposite problem — incontinence and loss of bladder control. For men with enlarged prostate glands, a common cause of bladder / urinary problems, drugs such as dutasteride (Avodart) and finasteride (Proscar) are available to stop the benign prostate growth or even shrink it. Medications that can relax the muscles of the bladder/urethra and also help with prostate enlargement include: alfuzosin (Uroxatral), doxazosin (Cardura), silodosin (Rapaflo), tadalafil (Cialis), tamsulosin (Flomax), terazosin (Hytrin). Medications should be viewed as only a short-term solution and not thought of as a permanent cure for urinary retention.
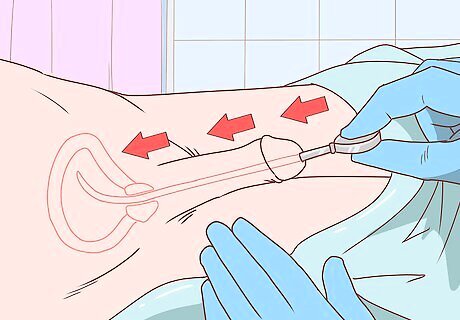
Think about urethral dilation and stenting. Urethral dilation treats a blocked urethra by inserting increasingly larger diameter tubes into the urethra to stretch it out. In contrast, a stent is also used to stretch out a constricted urethra, but the stent expands like a spring and pushes back the surrounding tissue with time, instead of being replaced by larger ones. Stents can be temporary or permanent. Both dilation and stenting are outpatient procedures that require a local anesthesia and sometimes sedation. Alternatively, the urethra can be made wider by inflating a small balloon attached to the end of a catheter. These procedures are performed by a genitourinary specialist called a urologist. Unlike regular catheterization which can be taught, dilation and stenting should not be done at home under any circumstances.
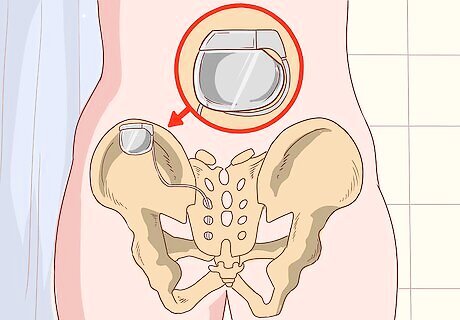
Consider sacral neuromodulation. Sacral neuromodulation, also called InterStim therapy, uses mild electrical pulses for the nerves that control the bladder and the muscles of the lower pelvis related to urinating. This therapy helps the brain, nerves and smooth muscles communicate better so the bladder can empty properly and at regular intervals. The electrical device has to be surgically inserted and turned on to function, but it's a reversible treatment that can be discontinued at any time by turning the device off or removing it from the body. This therapy is also known as sacral nerve stimulation, although the sacral nerves in and around the tail bone can also be stimulated manually by massaging the area with a vibrating device. Try this at home to see if it causes better bladder emptying. Sacral nerve stimulation is not indicated for a bladder or urinary retention problem caused by an obstruction. Be aware that not all forms of non-obstructive urinary retention can be treated with sacral nerve stimulation, so ask your urologist if it's a good idea for you.
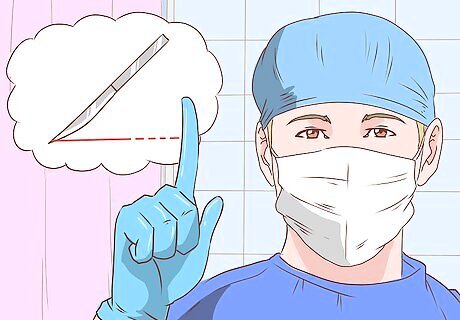
Consider surgery as a last resort. If all of the above-mentioned techniques and treatments don't help with your bladder / urinary problem, then surgery should be considered as a last resort if your doctor thinks it might be helpful. There are a variety of surgeries available, but it depends on the actual root cause of your problem. Some examples of surgical procedures to help with urinary retention include: an internal urethrotomy, a cystocele or rectocele repair for women, and prostate surgery for men. An internal urethrotomy involves repairing a urethral stricture (blockage) by inserting a special catheter with a laser on the end. A cystocele or rectocele procedure involves removing cysts, repairing holes and strengthening the vagina and surrounding tissues to move the bladder into its normal position. To treat urinary retention caused by benign prostatic hyperplasia (BPH), part or all of the gland is surgically removed, typically by the transurethral method (use of a catheter inserted through the urethra). Other surgeries can be done to remove tumors and/or cancerous tissues in the bladder or urethra if that applicable.


















Comments
0 comment